Glucose-6-Phosphate Dehydrogenase Deficiency in a Diabetic Patient with Discordant Hemoglobin HbA1c and Blood Glucose Measurements
Corentin Fontaine1*, Violeta Stojkovic1 and K Triches2
1Department of Laboratory Medicine, Hospital Center Bois De L'abbaye, Seraing, Belgium
2Department of Endocrinology, Hospital Center Bois De L'abbaye, Seraing, Belgium
- Corresponding Author:
- Corentin Fontaine
Department of Laboratory Medicine,
Hospital Center Bois De L'abbaye, Seraing, Belgium,
E-mail: c.fontaine@chba.be
Received date: December 27, 2022, Manuscript No. IPMCRS-22-15506; Editor assigned date: December 29, 2022, PreQC No. IPMCRS -22-15506 (PQ); Reviewed date: January 10, 2023, QC No. IPMCRS-22-15506; Revised date: January 20, 2023, Manuscript No. IPMCRS-22-15506 (R); Published date: January 27, 2023, DOI: 10.36648/2471-8041.9.1.258
Citation: Fontaine C, Stojkovic V, Triches K (2023) Glucose-6-Phosphate Dehydrogenase Deficiency in a Diabetic Patient with Discordant Hemoglobin HbA1c and Blood Glucose Measurements. Med Case Rep Vol.9 No.1:258.
Abstract
Hemoglobin A1c (HbA1c) is used as a parameter for diabetes diagnosis and follow-up. However, some haematologic conditions leading to premature destruction of red blood cells, as Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency could reduce HbA1c values. Therefore, in these cases, HbA1c measurement no longer adequately reflects average glucose level. We present a case where the discrepancy between HbA1c and blood glucose measurements allowed us to make an incidental diagnosis of G6PD deficiency.
Keywords
HbA1c; G6PD deficiency; Diabetes
Introduction
Hemoglobin A1c (HbA1c), a glycated fraction of Hemoglobin A, is a tool for diabetes diagnosis and monitoring. It reflects average plasma glucose over the previous 120 days, during erythrocyte lifespan. HbA1c is therefore used as a gold standard for glycaemic monitoring in diabetic patients. It is moreover an alternative for assessing glucose tolerance in people without diagnosed diabetes. Since 2011, the WHO recommends use of HbA1c as a diagnostic test for diabetes. A 6.5% HbA1c value is recommended as the cut-off, but values below 6.5% does not rule out the diabetes diagnosis using glucose tests [1]. As mentioned previously, HbA1c is a fraction of the Hemoglobin. Therefore, some hematologic conditions leading to shortened erythrocyte lifespan, such as a Glucose-6-Phosphate Dehydrogenase (G6PD) deletion, may result in a decrease in HbA1c. This decrease can lead to an abnormally low HbA1c level and the analysis may no longer adequately reflect the patient's glycaemic control. For example, approximately 2% of African Americans adults with diabetes can remain undiagnosed with HbA1c due to G6PD deletion [2]. We report a case of a diabetic patient with increased blood glucose level but with normal level of HbA1c (4.0%–6.0%) due to an incidental diagnosis of G6PD deficiency.
Patient Case
The patient is a man in his 50’s born in Italy. The patient has been living in Belgium for a year and a half when he had his first endocrinology consultation in our institution, in January 2017. He presented with type 2 diabetes diagnosed in 2004 in Sicily. His parents and siblings are all known diabetics. In his clinical history, there is a notion of ischemic heart disease monitored in cardiology. The clinical examination showed arterial hypertension and dyslipidaemia. The rest of the examination was unremarkable. The last biological check-up in November 2016 revealed a fasting blood glucose level at 186 mg/dL (71-100 mg/ dL). The most recent HbA1c Hemoglobin test, performed in December 2015, yielded a 6.4% (4.0%-6.0%). The patient has a distant notion of discordance between his HbA1c results and blood glucose levels, but knows no more about it. He is cared for in our diabetes ward and treated with metformin and insulin therapy (an average of 78 units per day). The patient was seen in consultations several times between February 2017 and September 2020, with an unremarkable clinical examination and stable weight. In September 2020, the ophthalmologist reported a decrease in visual acuity. Despite significant self-monitored blood glucose fluctuations, the HbA1c remained within normal values (Table 1).
The patient presented in October 2020 with consistently high morning blood glucose levels and a normal HbA1c. He was treated with dapaglifozine in an attempt to improve his blood glucose level, which were still too high. The patient was seen again in July 2021. Since the introduction of dapaglifozine, blood glucose values were significantly better but he described weakness and fatigue. Blood pressure was checked as normal. Dapaglifozine was stopped because of bad tolerability of treatment and a trial treatment with semaglutide was proposed in addition to insulin therapy. At the August 2021 consultation, semaglutide was well tolerated and allowed a remarkable evolution of the diabetes despite a significant reduction in insulin doses. In this context, a full letter was sent to the insurance company's medical advisor to request reimbursement for this drug. In fact, in order to be reimbursed for semaglutide in Belgium, the patient must fulfil the following requirements: “Patient with type 2 diabetes who, at the time of the first request, is insufficiently controlled (HbA1c>7.5%) after a treatment of at least 3 months with at least one anti-diabetic drug, including metformin”. Despite all explanations above, the medical advisor categorically refused reimbursement of semaglutide in view of the normal HbA1c values. In view of the refusal by the insurance company, after interpellation of the endocrinologist, we instigated the reason of the discordance in the laboratory.
According to our reference values, fasting glucose was always elevated (equal or above 126 mg/dL) while HbA1c was always normal (below 6.0%). Such a discrepancy between the hyperglycaemia and the HbA1c value was observed from the first sample in our laboratory (dated 08/05/2020) and confirmed with the following 4 samples (Table 1).
| Fasting glucose (mg/dL) | HbA1c (mmol/mol) | HbA1c (%) | |
|---|---|---|---|
| Techniques | Enzymatic technique (hexokinase/ G6PDH) on Alinity (Abbott®, USA) | High performance liquid chromatography on ADAMS HA-8180 (Menarini®, Italy) | |
| Reference values | 74-100, 100-126: Decreased glucose tolerance >126 (on 2 samples): Diabetes |
20.0-42.0 | 4.0-6.0 |
| 05-08-2020 | 175 | 30.1 | 4.9 |
| 02-02-2021 | 195 | 34.4 | 5.3 |
| 25-06-2021 | 126 | 27.9 | 4.7 |
| 22-11-2021 | 153 | 23.5 | 4.3 |
| 20-12-2021 | 141 | 24.6 | 4.4 |
Table 1: History of blood glucose and HbA1c results in our laboratory.
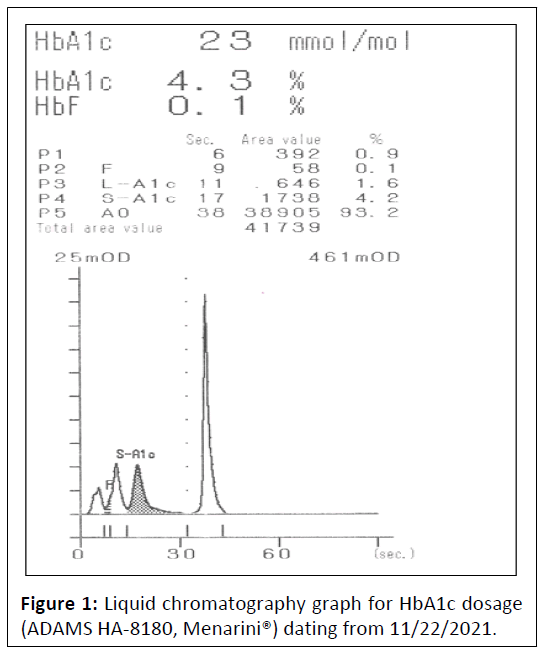
In order to explain this difference, the first step was to review the liquid chromatography graph for HbA1c dosage (Figure 1). The presence of a Hemoglobin variant or other interference was checked. However, the graph was in perfect agreement with the reported results and no anomalies were observed.
The next step was to confirm diabetes diagnosis with fructosamine test in November 2021. The obtained result was 178 μmol/L (122–236 μmol/L), which was within our normal values. Unfortunately, we could not rely on this result because the pathology was already stabilized by the treatment with semaglutide and insulin. Furthermore, we investigated haemolysis parameters: Haptoglobin was decreased at 0.28 g/L (0.40-2.40 g/L), reticulocytes were increased at 222.70 103/mm3 (25.00-120.00 103/mm3), but Hemoglobin remained within the normal range at 15.3 g/dL (13.5-16.9 g/dL). We also analyzed the erythrocyte morphology looking for spherocytosis, which was suspect, but the sample was 24 hrs old. Since the haemolysis parameters were positive and the presence of spherocytosis was suspect. A cryohaemolysis test and an Eosin-5'-Maleimide (EMA) staining were performed in order to confirm or refute the diagnosis of spherocytosis. Both were negative. We then drew a new blood sample in December 2021 and the suspect erythrocytic morphology was no longer observed. In this context of haemolysis with absence of spherocytosis, we looked for G6PD deficiency. We obtained a result of 1.4 UI/g Hb (9.4-18.2 UI/g Hb) and 0.10 (>0.7) for the G6PD measurement and the ratio respectively. We were therefore able to diagnose a G6PD deficiency with the possibility of haemolytic crises (between 10% and 30% activity). In 2022, the request to the insurance company for the reimbursement of semaglutide was reiterated with all new data, as this new treatment had led to a significant improvement in blood sugar levels. However, this new application was rejected again in regards to normal HbA1c results.
Discussion
The G6PD enzyme is involved in the pentose phosphate pathway and thus helps to protect red blood cells from haemolysis due to oxidative stress. A G6PD deficiency, especially in diabetic patients, leads to a premature destruction of red blood cells [3]. The HbA1c measurement no longer adequately reflects average glucose levels. Fructosamine level can be used as an alternative method to evaluate the average glucose level over the preceding 2–3 weeks and to monitor diabetic patients with G6PD deficiency [4]. Unfortunately, in our case, the fructosamine level was normal at the time of our investigation because the patient’s treatment has already been adjusted.
Most of G6PD-deficient patients have no clinical manifestations in the steady state and deficiency remains undetected until they are exposed to an exogenous haemolytic trigger such as bacterial or viral infections, ingestion of fava beans (favism) or drugs [3]. This could explain why our patient reached the age of 56 without diagnosis. Although this clinical situation is not considered as an indication for G6PD testing, in front of a discordance between glucose level and HbA1c, it is important to look for the presence of chronic haemolysis and if it is positive to carry out etiological investigations. The diagnosis is often quite simple and is based upon a combination of clinical history, family history, physical examination (splenomegaly, jaundice) and laboratory data (full blood count, RBC morphology, haemolysis parameters, reticulocyte count). Some additional and specific tests are available to confirm the diagnosis like G6PD dosage (G6PD deficiency diagnosis) or the EMA test (hereditary spherocytosis diagnosis).
We note that Chang et al. suggest that the fasting glucose/ HbA1c ratio is an alternative indicator of G6PD deficiency (but not thalassemia) in diabetic patients and could be used as a first tool for etiologic orientation of the discordance [5]. Moreover, the HbA1c levels can be affected by others factors listed by the WHO: Ineffective erythropoiesis altered Hemoglobin, impaired glycation, erythrocyte destruction and variability due to assays. Among those that could decrease HbA1c, the most frequent ones are Hemoglobinopathies, splenomegaly, hypertriglyceridaemia, and some drugs as antiretrovirals [1].
Actually, the discrepancy did allow us to make the fortuitous diagnosis of G6PD deficiency in our patient, as [6]. But a systematic diagnosis in this kind of clinical situation should still be evaluated like observed no significant difference in HbA1c levels between their diabetic patients with and without G6PD deficiency in Israel [7]. As there are no clinical manifestations of the G6PD deficiency, and that the haemolysis consists mainly of haemolytic crises, it would be interesting to verify, in this type of patient, if HbA1c could increase between these crises (which is not the case in our patient) and if the chronic haemolysis caused by G6PD deficiency decreases in a constant and sufficient manner the average life span of red blood cells and therefore HbA1c value.
Conclusion
This case shows abnormally low HbA1c values in a diabetic patient related to G6PD deficiency. To this date, our patient has no clinical complaints, and his diabetes is completely stabilized with a combination of metformin, insulin, and semaglutide. The purpose of this case is to describe a case of refusal of reimbursement of a drug due to normal HbA1c values. Reporting cases such as this one could add to the literature data on discordant measurements of Hemoglobin HbA1c and blood glucose and possibly lead to changes in reimbursement conditions in Belgium.
References
- https://apps.who.int/iris/handle/10665/43588
- Wheeler E, Leong A, Liu CT, Hivert MF, Strawbridge RJ, et al. (2017) Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: A transethnic genome-wide meta-analysis. PLOS Med 14: e1002383.
[Crossref], [Google Scholar], [Indexed]
- Roper D, Layton M, Rees D, Lambert C, Vulliamy T, et al. (2020) Laboratory diagnosis of G6PD deficiency, a british society for haematology guideline. Br J Haematol 189: 24-38.
[Crossref], [Google Scholar], [Indexed]
- Kosecki SM, Rodgers PT, Adams MB (2005) Glycemic monitoring in diabetics with sickle cell plus β-thalassemia hemoglobinopathy. Ann Pharmacother 39: 1557-1560.
[Crossref], [Google Scholar], [Indexed]
- Chang YS, Hsiao LY, Lin CY, Shih MC, Hsieh MC, et al. (2020) Fasting glucose-to-HbA1c ratio is a good indicator of G6PD deficiency, but not thalassemia, in patients with type 2 diabetes mellitus. Clin Chim Acta 506: 9-15.
[Crossref], [Google Scholar], [Indexed]
- Danzing J, Moser JT, Belfied P, Alter CA (2011) Glucose-6-phosphate dehydrogenase deficiency diagnosed in an adolescent with type 1 diabetes mellitus and Hemoglobin A1c discordant with blood glucose measurements. J Pediatr 158: 849-51.
[Crossref], [Google Scholar], [Indexed]
- Heymann AD, Cohen Y, Chodick G (2012) Glucose-6-phosphate dehydrogenase deficiency and type 2 diabetes. Diabetes Care 35: e58.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences