Cutaneous Lymphangioma Circumcriptum Successfully Treated with Cryotherapy
Ololade 1, Zacchaeus S2 and Olawore, Nureni O2
Ololade 1, Zacchaeus S2 and Olawore, Nureni O2
1Department of Chemistry, Faculty of Science, University of Medical Sciences, Ondo, Nigeria
2Department of Pure and Applied Chemistry, Faculty of Science, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
*Corresponding author: Zacchaeus S, Department of Pure and Applied Chemistry, Faculty of Science, Ladoke Akintola University of Technology, Ogbomoso, Nigeria, Tel No: 2348034836546; E-mail: zacchsnatpdt@gmail.com
Received date: December 21, 2020; Accepted date: January 12,2022; Published date: January19, 2022
Citation: Zacchaeus S (2022) Health Benefits of the Fruit Essential Oil of Eucalyptus Citriodora: Secondary Metabolites, Radical Scavenging, Antioxidant, Anti-inflammatory, Analgesic, Antimicrobial Potential. Int J Drug Discov Vol.8 No.1.
Abstract
Lymfangioma circumscripptum is superficial malformation, presenting as micro to macraoscopic vesicles. It is often disfiguring and can negatively affect one’s quality of life due to complications such as infection, and pain, making it of high value to elucidate current treatment options for the condition. High recurrence rates and a risk of scarring make lymphangioma circumscriptum difficult to treat. Treatment options for lymphangioma circumscriptum there are surgical excision, laser therapy, sclerotherapy, cryotherapy, radiotherapy, electrocautery, electrodessication and imiquimod in treating lymphangioma circumscriptum. In this case we treating lymphangioma circumscriptum using cryotherapy to minimal adverse effects.
Keywords: Lymphangioma, Cryotherapy, Cystic Tumor
Introduction
Cutaneous lymphangioma circumscriptum (CLC) is a rare congenital malformation of the superficial cutaneous lymphatic ducts, which manifests isolated or associated with deep lymphangioma or angiodysplastic syndromes. This lymphangioma is characterized by changes in the lymphatic structures with the formation of subcutaneous cisterns and ectopic vessels interconnected through dilated ducts that project into the skin in the form of superficial vesicles with thin walls and variable color[1-3].
A variety of treatment options for lymphangioma circumscriptum include surgery, sclerotherapy, cryotherapy, and lasers. Although these treatment options may yield positive results in some cases, relapses are often reported due to the deep placement of the lesions. Here, cases of cutaneous lymphangioma circumscriptum successfully treated with cryotherapy are presented.4,5
Case
A 22-year-old female came to the dermatology outpatient clinic of Dr.
Sometime General Hospital Surabaya on March 06th 2019. She came with
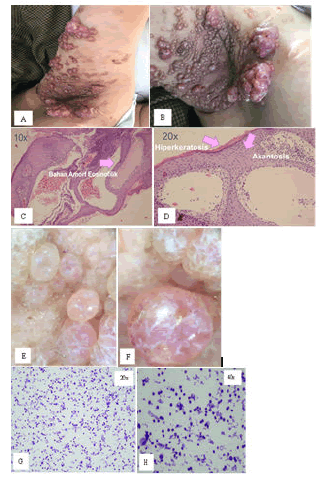
chief complaint of multiple vesicles on her right axillar. Her parents complained about it since she was 10 months old. Firstly, when she was 10 months old there are multiple vesicles in her right axillar. When she was 16 months old the multiple vesicles are surgically removed in Kediri Hospital, but when she was 10 years old vesicles reappear. In 2005 when she was 13 years old vesicles began to increase and more wide. In the last 2 years in 2017 clear liquid came out from vesicles cluster. Since 2018 clear liquid has been release especially if she is in activity. At the beginning of the year 2019 pus starts coming and made a bad smell (Fig. 1 A-B). Because of feeling uncomfortable of this condition, March 06th 2019 she sought out help to dermatology and venereology outpatient clinic of Dr. Soetomo General Hospital out dermatology and venereology. Patients hospitalized to treat secondary infections of her illness and wound treatment to reduce pus and bad smells
The physical examination of general state was all within normal limit. Blood pressure was 120/80 mmHg, pulse rate was 80 times per minute, respiratory rate was 20 times per minute. From head and neck, there were no signs of anemia, cyanosis, icterus, or dyspneu. From thorax examination, heart and lungs were normal. From abdomen, liver and spleen were not palpable. From her upper and lower extremities there were no edema and warm on palpation.
Dermatological examination on her right axillar region discovered multiple nodule eritematosa, with varying sizes, some vesicles and there were exudative clear fluid and pus (Fig. 1 A-C). The laboratory examination on March 06th 2019 was revealed: haemoglobin was 14,0 g/dL, white blood count 11.090/mm3, thrombocyte 302.000/L, and hematocrite 41,2%. Microscopic findings from gram staining examination result luekosit 4-6, epitel 1-2, coccus gram positive 2. Blood culture examination result Pseudomonas aeruginosa, we gave oral therapy with clindamycin to reduce secondary infection.
Histological examination of the vesicle was revaled hyperkeratosis and acanthosis in the epidermis layer. several lumen which is covered by a layer of endothelial cells containing eosinophilic amorphous material. Stroma is fibrous connective tissue with infiltration of neutrophil, lymphocyte, histocyte, and plasma cell inflammation in the dermis layer. There are no signs of malignancy and the conclusion according to lymphangioma sirkumskripta (Fig. 1 C-D).
Dermoscopy showed yellow lacunae surround by pale septa without inclusion of blood, and yellow to pink lacune dark-red or bluish lacunae. The picture of dermoscopy can be clearly seen on the Figure 4 below. The conclution dermoscopy described as CLC. Fine needle aspiration biopsy showed Hypocellular smear contains the spread of mononuclear inflammatory cells and macrophages. Eosinophilic background. Conclusion benign lession suggests a lymphavascular lesions (Fig. 1 E-H).
Based on these findings, from physical examination, histophatology and dermoscopy. The diagnosis of cutaneous lymphangioma circumscriptum was established. Treatments for this patient treated with cryotherapy (Fig. 2 A-C). After 6 treatments with cryotherapy every 2 weeks we observed no development of new lesions, vesicles and nodules are reduced (Fig. 3 A-C).
Discussion
Lymphangiomas are congenital malformations, hamartomatous of the lymphatic system that may involve the skin and subcutaneous tissues. They can occur on any cutaneous surface or mucous membrane. The most common skin sites are the head and neck, proximal extremities, buttocks, and trunk, while the intestines, pancreas, and mesentery are other potentially affected organs. Their skin involvement ranges from small and well demarcated malformations to large, diffuse ones with unclear borders [6-8].
Diagnosis of this case based on clinical features, dermoscopy and histopathology examination. Frim clinical features cutaneous lymfangioma, is characterized by persistent, multiple cluster of translucent vecicles that usually contain lymph fluid. Dermoscopy findings red and pale homogenous area resembling vascular lagoons and whitish and yellowish areas with thin linear vessels. Histophatology findings acanthosis, hyperkeratosis, and multiple dilated lymph vessels.
In 1877, Wegener classified lymphangiomas into three major groups: simple, cavernous, and cystic. Cutaneous lymphangioma circumscriptum (CLC), part of the simple group, was described by Fox and Fox in 1878. They named it ‘‘lymphangiectodes’’ It was renamed in 1889 to ‘‘lymphangioma circumscriptum’’ by Morris. Currently, however, lymphangiomas are divided into two major groups, superficial and deep, based on the depth and size of the abnormal lymph vessels. The superficial group includes CLC, whereas the deeper group includes cavernous lymphangiomas and cystic hygromas. The lym- phangiomas of the deeper group were once considered independent entities, but currently cystic hygroma is believed to be an aneurysmic variant of cavernous lym- phangioma. It is possible for both groups to appear in the same patient. CLC is the common form of cutaneous lymphangiomas, one that may recur if improperly excised [7-10].
Lymphangiomas are uncommon, accounting for 4% of all vascular tumors and about 25% of all benign vascular tumors in children. The incidence rate of lymphatic malformations is 1.2–2.8 per 1000 live births in the United States. About 50% of these are apparent at birth; 90% appear by appear by 2 years of age.
This is related to my patient she complaint since she was 10 months old. Gender differences have not been noted, except in a few reports in which females predominated males. Lymphangiomas may appear spontaneously in adolescence or adult life. No correlation among CLC, mucous membrane lymphangioma, or internal organ lymphangioma was found in a study by Flanagan et al. No familial histories of lymphangioma were noted either. Robust epidemiological evaluation may prove valuable [10,12].
The pathogenesis of CLC was described in 1976 by Whimster et al. During development, abnormal lymphatic cisterns grow separately from normal lymph vessels in the deep subcutaneous tissue. These reservoirs may be a byproduct of a primitive lymphatic sac that has improperly connected with the rest of the lymphatic system. The cisterns have channels that allow them to communicate with ectopic lymph vessels. Contractions of the smooth muscle lining these cisterns will cause the abnormal ectopic lymph vessels to dilate and protrude from the skin [11,13].
Regardless of the visible CLC size, the deep cisterns feed the surface lymphangioma. This is analogous to an ice- berg, where more lymphatic involvement is below the surface of the skin. Whimster’s observations are supported by those of lymphangiographic and radiographic studies. They reveal that large multilobulated cisterns extend deep in the dermis and laterally beyond the obvious clinical view. The deep cisterns show no evidence of communication with the adjacent normal lymphatics. The absence of skin lymphedema further supports the presence of normal functioning lymphatics. The reason these primitive lymph sacs do not connect to the rest of the lymphatic system is unknown [14,15].
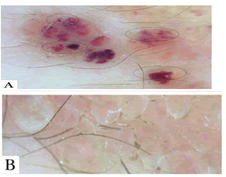
Cutaneous lymphangioma circumscriptum is typically seen as a small number of translucent cutaneous vesicles at or soon after birth, although possible at any age. They may range in size from minute vesicles to larger bullae. Specifically, 2–4 mm clusters of vesicles with pink, red, or black discoloration as a byproduct of hemorrhage are common. These vesicles often resemble frog spawn and tend to increase in number and size with occasional rupture leading to bleeding or drainage. Underlying lymphatic vessels occupy the dermal papilla and push upward against the epidermis, leading to a saccular appearance of the vesicles. CLC can also be found with hyperkeratosis and or verrucous changes, mimicking a warty appearance (Fig. 4 A-B).
The sites of predilection are the proximal extremities, trunk, axilla, and oral cavity, especially the tongue, but CLC may also occur on the penis, vulva, and scrotum [14-17]. This is related to my patient she complaint multiple nodul eritematosa, with varying sizes, some vesicles.
Cutaneous lymphangioma circumscriptum was divided into two main groups, classic and localized, by Peachey and Lever in the 1970s. Although their clinical appear- ance is similar, the size, distribution, histology, and asso- ciated symptoms differ greatly between the two groups. According to Peachey et al., the classic form presents at or soon after birth and is often larger than a square centi- meter. Sometimes a diffuse and palpable subcutaneous swelling is detectable before the appearance of vesicles. In classic CLC, it is uncommon for areas originally vesicular to become thick and develop warty plaques. Classic CLC usually occurs over the proximal part of the limbs, especially involving the upper arm, axilla, adjacent chest, and scapular regions. Localized swelling is often detectable in areas adjacent to the vesicles. The localized form, however, is seen at any age, is often <1 cm2, and can appear anywhere on the body. In Peachey’s original study, 25% of patients were older than 45 years of age when present- ing with the local form of CLC. Localized CLC usually does not present in the same regions as classic CLC. Cases with overlap of the two forms exist. In both forms, there is no evidence of the abnormal deep lymphatics communicating with the normal lymphatics [18].
Dermatoscopic examination of CLC shows a lacunar / saccular pattern. Presence of clear fluid appears as light brown lacunas with pale septa. If blood has infiltrated in a patchy manner, scattered areas of redness appear within the lacunas. However, if there is homogeneous distribution of blood in the CLC, a pink hue overwhelms the lacunar structures (Figure 9 A-B). With marked blood presence in the CLC, dermatoscopic findings are indistinguishable from those of hemangiomas (Table 2) [19].
Lymphedema of the lower limb is also associated. CLC was identified in patients with concurrent cystic hygroma, possibly suggesting a general- ized developmental disorder of the lymphatic system. Other common complications include cellulitis and bleeding. Involvement of unusual locations, such as the scrotum and viscera, may occur. Associations between lymphangioma and other conditions such as the Proteus, Cobb, and Maffucci syndromes were reported [20].
Malignant transformation of CLC is rare. A minute number of lymphangiosarcomas were noted on sites of CLC with prior radiation therapy. A Dabska tumor, or papillary intralymphatic angioendothelioma, was reported forming within an adolescent patient’s CLC. The lymphangioma recurred after excision, but the Dabska tumor did not. Squamous cell carcinoma has been described arising within CLC.21
| Dermatoscopic appearance | Underlying pathology |
|---|---|
| Lacunar/saccular pattern of light brown lacunae with pale septa | CLC with clear fluid |
| Redness within lacunae | Minimal blood extravasation in CLC |
| Diffuse pink hue with pale septa | Modest blood contamination in CLC |
| Marked redness resembling hemangioma | Significant blood contamination in CLC |
Table 1: Dermatoscopic features of cutaneous lymphangioma circumscriptum (CLC).
Figure 5: a) Dermoscopy - Red and pale homogenous areas resembling vascular lagoons. In some, a raised surface appeared due to the sedimentation of blood according to their corpuscles density, leading to a color transition from dark to light in some lacunae –Hypopyon-like (circles). b) Dermoscopy – Whitish and yellowish lacunar areas with thin linear vessels
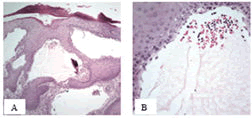
The vesicles of CLC represent an overpopulation of dilated lymphatic channels expanding within the papillary dermis. They can be associated with overlying hyperkeratosis and acanthosis and may possess capillary tufts. These lymphatic channels are numerous in the papillary dermis and often extend below to the reticular dermis or subcutaneous tissue. The deepest vessels with which the CLC vesicles communicate tend to have a larger caliber and a thick wall composed of smooth muscle (Fig. 6 A-B) [21,22].
Upper dermal vessels have a wide lumen, whereas deep dermal vessels have a narrow one. The lumen of all involved vessels is filled with lymphatic fluid and often red and white blood cells. The mechanism of red blood cell extravasation into the dilated lymphatics is unknown, but microshunts between capillaries and smaller lymphat- ics may be one source. The communicating channels are lined by flat endothelial cells which stain positive for Ulex europaeus agglutinin-1, a well known plant derived marker of endothelial cells. Markers including lymphatic vessel endothelial receptor 1 and vascular endothelial growth factor C are helpful in distinguishing lymphatic endothelial cells from those of blood vessels. The dermis often has numerous lymphocytes and shows evidence of fibroplasia.23
This patient from histological examination also was reveled hyperkeratosis, acanthosis, vesicles containing of red cells in its fluid. Result from dermoscopy evamination reveled whitish and yellowish lacunar with thin vessel also there are res and pale homogenous areas resembling vascular lagoon.
Ultrastructural analysis of lymphatic vessels of the upper and deep dermis demonstrates important differ- ences. Endothelial cells of the upper dermal lympha- tic vessels show higher electron density, are flattened (0.1–1.3 lm), and possess a well developed and partially multilayered basal lamina. The nuclei of the cells are oval or occasionally indented with peripherally condensed chromatin. The endothelial cells of the deep dermal lym- phatic vessels are less flat (0.6–2.5 lm) and are separated from connective tissue by discontinuous basal lamina. The nucleus is slightly flattened with normal appearing chromatin. The cells of the deep dermal lymphatic vessels also have pinocytotic vesicles, formed from cell membrane invagination, which are not found in the cells of the upper dermal lymphatic vessels [24].
The differential diagnoses of CLC include the diseases listed in Table 3. Lymphangiectasis and metastatic carcinoma of the skin are notable Cutaneous metastasis of internal malignancy is particularly worrisome, as it may be a presenting sign of cancer. This entity often arises as a non-specific painless dermal or subcutaneous stony nodule with an intact epidermis that is flesh-colored, pink, violaceous, or brown– black. Violaceous papulovesicles that resembled CLC may be noted in telangiectatic metastatic breast carcinoma. Cutaneous metastasis occurs in 0.7–9.0% of all patients with cancer. CLC may resemble lymphangiectasis, a condition induced by lymphatic obstruction. In lymphangiectasis, previous surgery or radiation therapy has often been performed in the affected area, resulting in identical histology as CLC but a different pathogenesis. Smaller CLC can resemble warts, molluscum contagiosum, hemangioma, angiokeratoma, or lymphangioendothelioma [24,25].
| Diagnosis | Appearance | Distribution |
|---|---|---|
| Cutaneous lymphangioma circumscriptum | Scattered or grouped vesicles ranging from minute to >5 mm overlying normal skin or papules. Plaque-like or warty hyperkeratosis possible. Colors range from clear, pink, red, purple, or black | Proximal part of limbs (classic form) or all cutaneous surfaces (localized form) |
| Lymphangiectasis | Fluid-filled vesicles ranging from clear to smooth, flesh-colored nodules | All cutaneous surfaces, often appearing along an incisional scar |
| Cutaneous metastasis (carcinoma telangiectoides) | Nodules - often nonpainful, round or oval, firm, mobile, and rubbery. Flesh colored to brown, blue-black, or red and purple. Sizes ranging from minute to large tumors | Often near the site of primary tumor |
| Hemangioma | Hypopigmented macule ranging to a bruise-like, red, or blue macule. Strawberry like or nodular violaceous forms possible | Head and neck most common, followed by trunk, lower extremities, and upper extremities |
Table 2: Characteristics of cutaneous lymphangioma circumscriptum and selected differential diagnoses
There is no pharmacologic treatment for CLC. The main considerations are cosmetic outcome, continued lymphatic and blood leakage, pain, swelling, and persistent superinfections. Antibiotics are used for secondary infections, primarily Staphylococcus aureus. Surgical excision is the approach of choice for primary treatment of lymphangiomas. The objective is to remove as much of the lymphangioma as possible so as to avoid recurrence. Excision should be through the full thickness of skin and subcutaneous tissue and down to the deep fascia until normal subcutaneous tissue is exposed. This eliminates the abnormal hypertrophied lymphatic cisterns which serve as sites of recurrence. Frozen section analysis of the lateral and deep sections ensures clear margins. If confined to the superficial dermis, the malformation is more amenable to surgery and possesses longer lasting results.25 In this case treated with cefadroxil to treat secondary infections and cryotherapy. After 6 treatments with cryotherapy every 2 weeks we observed no development of new lesions, reduced vesicles and nodules.
Cryotherapy has been reported 75% good out comes to reduction in the size of an CLC lesion after 5 session of Cryotherapy 2 week intervals.25 In this case after 6 treatments with cryotherapy every 2 weeks we observed no development of new lesions, reduced vesicles and nodules. In this case patient still need cryotherapy treatment 2 week intervals until there is no more lesion.
Radiation therapy should be avoided, as malignant conversion is possible. Sclerotherapy with hypertonic saline may be successfully employed. In multiple cysts the technique was only useful as a presurgical adjunct.25 This patient also show good result treated with cryotherapy after 6 times treatment vesicle and nodule are reduces and there no comes fluid from the lesion.
Conclusion
In summary, we can conclude that cutaneus lymphangioma circumscriptum (CLC) is a rare congenital malformation of superficial cutaneous lymphatic duct. The clinical dermatoscopy and histopathological correlation is great importance. The objective is to remove as much of the lymphangioma as possible so as to avoid recurrence. Cryotherapy, have been utilized with good outcomes. Cutaneus lymphangioma circumscriptum is an evolving situation with ongoing discoveries and further research needs.
References
- Wiegand S, Eivazi B, Barth PJ (2008) Pathogenesis of lymphangiomas. Virchows Arch 453: 1-8.
- Bauer BS, Kernahan DA, Hugo NE (1981) Lymphangioma circumscriptum. A clinicopathological review. Ann Plast Surg 7: 318-326.
- Fox T FT (1878) On a case of lymphangiectodes with an account of the histology of the growth. Trans Pathol Soc London 30:470-476.
- Morris M (1889) Lymphangioma Circumscriptum. Unna PG, M. London: Lewis .
- Filston HC (1994) Hemangiomas, cystic hygromas, and teratomas of the head and neck. Semin Pediatr Surg 3:147-159.
- Flanagan BP, Helwig EB Cutaneous Lymphangioma. Arch Dermatol 113:24-30.
- WHIMSTER IW. The pathology of lymphangioma circumscriptum. Br J Dermatol. 1976;94:473-486. \
- MartÃnez-Menchón T, Mahiques-Santos L, Febrer-Bosch I, Valcuende-Cavero F, Fortea-Baixauli JM. Lymphangioma circumscriptum: An example of Whimsterâ??s hypothesis. Pediatr Dermatol. 2004;21:652-654.
- Mordehai J, Kurzbart E, Shinhar D et al. Lymphangioma circumscriptum. Pediatr Surg Int. 1998;13:208-210.
- Erkiliç S, Koçer NE, Mutaf M. Giant lymphangioma circumscriptum mimicking wart in a 13-year-old girl [3]. J Dermatol. 2006;33:501-503.
- Horn LC, Kühndel K, Pawlowitsch T, Leo C, Einenkel J. Acquired lymphangioma circumscriptum of the vulva mimicking genital warts [2]. Eur J Obstet Gynecol Reprod Biol. 2005;123:118-120.
- Yagmurlu A, Gokcora IH, Duran E, Gollu G. A childrenâ??s disease of rarity: â??Scrotal Lymphangioma Circumscriptum.â?ÂÃÂ Int Urol Nephrol. 2004;36:229-233.
- Yildiz F, Atahan IL, Ã?zyar E, et al. Radiotherapy in congenital vulvar lymphangioma circumscriptum. Int J Gynecol Cancer. 2008;18:556-559.
- Peachey RD, Lim CC WI. Lymphangioma of skin. A review of 65 cases. Br J Dermatol. 1970;83:519-527.
- Lever W S-LG. Histopathology of the Skin. Philadelphia-Toronto: J.B. Lippincott Co; 1975.
- Arpaia N, Cassano N, Vena GA. Dermoscopic features of cutaneous lymphangioma circumscriptum. Dermatologic Surg. 2006;32:852-854.
- Wolf IH. Dermoscopic diagnosis of vascular lesions. Clin Dermatol. 2002;20:273-275.
- EJ B (1988) Lymphangioma circumscriptum. J Dermatol Surg Oncol 14:1033.
- Irvine AD, Sweeney L, Corbett JR. Lymphangioma circumscriptum associated with paravesical cystic retroperitoneal lymphangioma. Br J Dermatol. 1996;134:1135-1137. 20.
- Child FJ, Werring DJ VA (1998) Proteus syndrome: diagnosis in adulthood. Br J Dermatol. 139:132-136.
- Shim JH, Lee DW, Cho BK (1996) A case of cobb syndrome associated with lymphangioma circumscriptum. Dermatology 193:45-47.
- Samlaska CP, Levin SW, James WD (1989) Proteus syndrome. Arch Dermatol 125:1109-1114.
- King DT, Duffy DM, Hirose FM, Gurevitch AW (1979) Lymphangiosarcoma Arising From Lymphangioma Circumscriptum. Arch Dermatol 115:969-972.
- Emanuel PO, Lin R, Silver L, Birge MB, Shim H, Phelps RG. Dabska tumor arising in lymphangioma circumscriptum. J Cutan Pathol. 2008;35:65-69.
- Schwartz RA, Dabski C, Da̧bska M (2000) The Dabska tumor: A thirty-year retrospect. Dermatology 201:1-5.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences