Bilateral Internal Carotid Agenesis - Incidental Diagnosis in 5 Year old Pre-Schooler
Polet Portillo-Cálix, Alison Miralda-Cálix, Aarón Mejía-Fúnez and Carlos Figueroa-López
DOI10.21767/2471-8041.1000026
Carlos Figueroa-López1, Alison Miralda-Cálix2, Aarón Mejía-Fúnez3 and Polet Portillo-Cálix4*
1Pediatric Specialities, María Hospital, Tegucigalpa, Honduras
2Medical Clinics Hospimed, Tegucigalpa, Honduras
3Santa María Clinic, Reitoca Francisco Morazán, Honduras
4Dirección de Medicina Forense/Ministerio Público, Tegucigalpa,Honduras
- *Corresponding Author:
- Polet Portillo-Cálix
Forensic Physician, Dirección de Medicina Forense/Ministerio Público, Tegucigalpa, Honduras
Tel: 50498388422
E-mail: alejapolet@hotmail.com
Received date: May 28, 2016; Accepted date: June 22, 2016; Published date: June 27, 2016
Citation: Figueroa-López C, Miralda-Cálix A, Mejía-Fúnez A, et al. Bilateral Internal Carotid Agenesis - Incidental Diagnosis in 5 Year old Pre-Schooler. Med Case Rep. 2016, 2:3.doi: 10.21767/2471-8041.100026
Abstract
Bilateral internal carotid agenesis is a rare congenital malformation, poorly documented in the literature. We report the case of a 5 year old patient with an incidental diagnosis of this entity, after an evaluation of an open craniocerebral trauma and post-traumatic seizures. Patient diagnosis was performed by a magnetic resonance angiography showing no reflux of internal carotid arteries (bilateral agenesis) and an increase in the caliber of vertebral and basilar arteries.
Introduction
Agenesis of the internal carotid artery (ICA) is defined as the failure in the development of this structure and the complete absence of the carotid canal. It is considered a rare anomaly, with an incidence lower than 0.01% [1-3], usually presented as unilateral involvement, predominantly on the left side (3/1) and exceptionally presented bilaterally, there are currently only 26 documented cases of bilateral agenesis worldwide in literature [2,3]. In most cases patients remain asymptomatic for long periods of time due to the development of compensatory collateral circulation through the circle of Willis or persistent embryonic arteries, which can be sufficient to maintain cerebral perfusion, without ruling out possible limitations and complications of this adaptation of the vascular system [1]. The first documented case was described by Tode in 1787 after performing a necropsy, and the first diagnosis "in vivo" was conducted by Verbiest in 1954 through cerebral arteriography [2].
The diagnosis is primarily made incidentally during a radiological examination by other causes, for example, after a cerebrovascular event such as a subarachnoid hemorrhage subsequent to the rupture of an aneurisma [3]. The etiology of the abnormalities of the internal carotid artery is controversial, in general terms, among the causes of these changes are considered abnormal embryological development and loss of elasticity of the vessels with age, and however major alterations and those found in children are attributed to congenital malformation [4].
The aim of this publication is to present the first reported case of this entity in Honduras and one of the few reported in World scientific literature, diagnosed incidentally on brain radiologic evaluation with secondary posttraumatic seizures.
Case Report
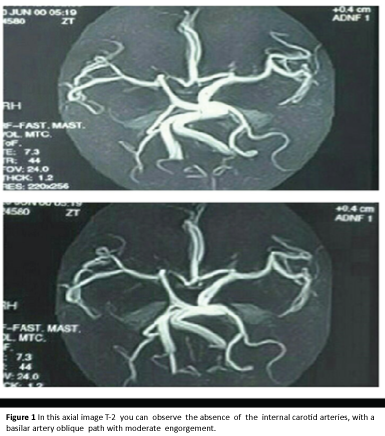
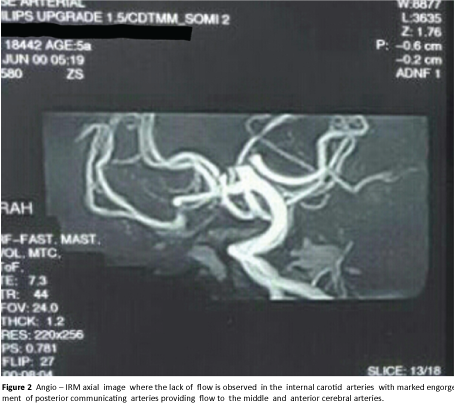
Male patient 5 years old from a rural area of Honduras, with a history of having suffered trauma in the frontal region of the skull, secondary to blunt blow by precipitation of a different plane lift of approximately 1 meter high, without loss of consciousness, and intense holocraneal headache; without medical attention for it, coming two days later to a private medical clinic with a 38ÃÆáÃâõÃâââ¬â¢C fever diagnosed with right middle ear infections, treated with first-generation cephalosporin (cefadroxil) and analgesic (paracetamol), being evaluated again the following 2 days by clonical tonic generalized seizures lasting from two to three minutes, with oculogyration, salivation, cyanosis, loss of consciousness (there were no personal or family history of epilepsy), being referred to pediatric emergency services of the Hospital School University (Hospital Escuela Universitario) located in the capital city, Tegucigalpa. The patient was admitted with a diagnosis of traumatic brain injury (TBI) opened by right hemotympanum and secondary convulsive syndrome, Glasgow coma scale of 10 points. Interconsultation with otolaryngology service was performed, extracting foreign body (bean seed) from the ear, thus discarding hemotympanum. The patient again presented seizures with similar characteristics, treated with phenytoin and diazepam. Pediatric neurosurgery service asked for computerized brain tomography (CT), which showed a dilated interpeduncular cerebral cistern, hyperintense nodular image on the left side and normal bone structures. Thus, angio magnetic resonance was requested, reporting: hyper intense nodular cortical areas in T2 and Flair compatible with areas of bilateral occipital bruising, no reflux of internal carotid arteries, engorgement and flexibility of vertebral and basilar arteries as well as the posterior communicants, giving a diagnosis of bilateral agenesis of the internal carotid arteries. The patient showed improvement in clinical symptoms only with phenytoin and was discharged on the seventh day, now in semi-annual follow-up for 2 years from the service of pediatric neurology, treated with amitriptyline and phenytoin orally, with no recurrence of posttraumatic seizures (Figures 1 and 2).
Discussion
The circle of Willis is a vascular system that provides the cerebral blood circulation which is divided into anterior and posterior circulation; the first provided by the internal carotid arteries which provide the highest blood flow and the second by the vertebral arteries; This vascular circuit interconnects the supraclinoid portion of both internal carotid, horizontal segment of the anterior cerebral arteries and the horizontal segment of the posterior cerebral arteries through the anterior communicating and posterior communicating arteries respectively, introducing variations in their normal anatomy in up to 60% of cases [5,6]. Embryonic development of the internal carotid artery (ICA) is defined in its caudal portion by third gill arch and cranial portion by the dorsal aorta, then between the third and fifth week of embryonic development a handle is formed. This handle connects these segments and completes its development for the sixth week.
Alterations in the development of internal carotid artery are extremely rare, they can have variations in their morphology, such as curliness or tortuosity which mainly affect the cervical portion or major congenital anomalies such as agenesis; which corresponds to the complete lack of development of the structure, aplasia; which it refers to the absence of development, but its predecessor did exist and hypoplasia incomplete development [4,7] when these occur usually unilateral and three times more common in left side.
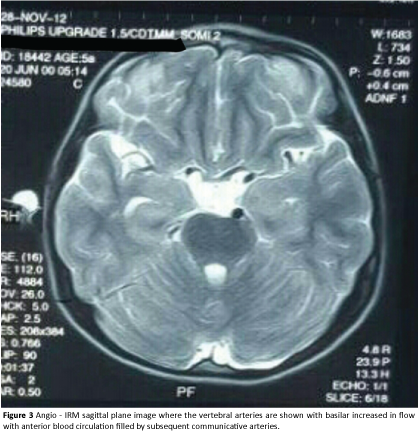
Within these anomalies the postulated causes for unilateral absence of the internal carotid artery have been focused on mechanical and hemodynamic stress in the embryonic stage, including defects related to the exaggerated folding of the embryo to one side and amniotic band constriction. So far, no explanation for a bilateral absence is known but it is related to more serious complications [7]. Although in our case a serious secondary complication has not yet been presented or demonstrated (Figure 3).
Unilateral agenesis of the internal carotid artery is commonly asymptomatic under normal conditions due to the fact that in these cases the contralateral artery supplies partially or totally the vascular territory and in case of a bilateral agenesis flow is compensated mostly through the vertebral arteries [8] as presented in our case where the absence of both internal carotid arteries is compensated through the vertebral arteries, basilar and posterior cerebral arteries, the imaging study reports where dilation is observed in these arteries. In the absence of both internal carotid arteries, according to image study reports, shows an expansion of the vertebral arteries, basilar and posterior, as a compensatory response to the anomaly.
The diagnosis of this disorder is usually casual, since the patient consults for symptoms such as headache, blurred vision, paralysis of some cranial nerves, epilepsy, hemiparesis, Bernard-Horner syndrome and even as an incidental finding in traumatic brain injury, part of the diagnosis process of these patients are imaging studies in which agenesis of one or both ICA is diagnosed and in many cases there is no relationship with the symptoms mentioned before. In the case we are reporting the patient comes for repetitive seizures secondary to a trauma and as an incidental finding the diagnosis of bilateral carotid agenesis is given, without knowing whether this or the trauma are the cause of the pathology.
Imaging studies used for diagnosis of this anomaly are: cerebral angio-tomography, computed axial tomography, magnetic angioresonance and cerebral 3-D angio-resonance which allows fully evaluating all structures of the cerebral vascular system and thus not overlooking other findings such as aneurysms. In these studies alterations in the caliber of the arteries can be observed, abnormal vascular communications, evidence of hemiatrophy in the affected side of the brain and even the absence or decrease in the size of the carotid canal at the cranial base [9,10]. In our case the definitive diagnosis was by magnetic angio-resonance, after helical computed tomographic findings being inconclusive.
Agenesis of the internal carotid, being a rare anomaly without specific symptoms can be overlooked in most cases but when this occurs, an incidental finding usually happens; this can lead to the development of severe complications such as: aneurysms and strokes that lead to a followed up by brain magnetic resonance angiography periodically in order to reduce the risk of future complications and timely treat those secondary surgical pathologies to this malformation.
References
- López-Alvarez F, Bernardo-Corte J, Gómez-Martínez R, Suarez-Nieto C (2012) Agenesia unilateral de arteria carótida interna.Acta Otorrinolaringol63:72-74.
- Escobar B, BenitezVasquez M, Redondo P, Meilán Martínez A, SantamartaLiebana E, et al. (2012) Ausencia congénita de la carótida interna. Seram 1-22.
- Da Paz Oliveira G, Rezende Soares L, Paz G, Pessoa Vale B (2014) Agenesia bilateral de arteria carótida interna: relato de caso. J VascBras 13: 336-339.
- Ortega F, Mena G, Ribalta L (2009) Caso clínico radiológico: carótida interna aberrante. RevMedClin Condes 20:549–551.
- Hassan A, Hassan S, Kaul N, Ghulam (2013) Right internal carotid agenesis: A rare case anatomical, neurosurgical and radiological perspective. GJMR 13:37-39.
- Gonzales X, Landó F (2014) Angiotomografia cerebral: variantes anatómicas más frecuentes del polígono de Willis, ensayo iconográfico. Rev. Imagenol 17: 93–97.
- Huang-Hellinger F, Baker D, Chepuri B, Pearse Morris P (2001) Congenital absence of the internal carotid artery: Case reports and review of the collateral circulation. AJNR Am J Neuroradio 22: 1953–1959.
- OrakdÃÆââ¬ÅÃâçÃÆââ¬Â¡Ãâçen M, Berkman Z, ErÃÆÃâ Ãâââ¢ahin M, BÍber N, Somay H, et al. (2007) Agenesis of the left internal carotid artery associated with anterior communicating artery aneurysm: A casereport. TurkishNeurosurgery 17: 273-276.
- Yadav P, Kumar A, Saili A, Datta V (2009) Congenitalhypoplasia of the internal carotid artery. Indian J Pediatr 76: 1061-1062.
- Neves W, Kakudate M, Cêntola P, Garzon G, Agua A, et al. (2008) Agenesis of the internal carotid artery: A case report. RadiolBras41:63–66.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences