Aspergillus fumigatus in A Fine Needle Aspiration of a Cavitary Lung Lesion
Ziyan T Salih and Avinash K Shetty
DOI10.21767/2471-8041.100086
Ziyan T Salih1* and Avinash K Shetty2
1Department of Pathology, Wake Forest Baptist Medical Center, Medical Center Boulevard, USA
2Department of Pediatrics and Infectious Disease, Wake Forest Baptist Medical Center, Medical Center Boulevard, USA
- *Corresponding Author:
- Ziyan T Salih
Assistant Professor, Department of Pathology
Wake Forest Baptist Medical Center
Medical Center Boulevard, Winston-Salem
NC 27157, USA
Tel: +44 121 424 2000
E-mail: zsalih@wakehealth.edu
Received Date: September 25, 2017 Accepted Date: October 24, 2017 Published Date: October 26, 2017
Citation: Salih ZT, Shetty AK (2017) Aspergillus fumigatus in A Fine Needle Aspiration of a Cavitary Lung Lesion. Med Case Rep Vol.4 No.1:51. doi: 10.21767/2471-8041.100086
Abstract
Fine needle aspiration cytology (FNAC) can be quite helpful in distinguishing malignancy from infection. Fungal elements may be detected using routine stains as in our case. The present case describes a 64-year-old male presented with chills and mild dyspnea on exertion after completing four cycles of chemotherapy for stage IIA adenocarcinoma of the lung. Use of special stains to enhance cytomorphological changes in conjunction with microbiology culture results is critical to identify the specific microorganism.
Keywords
Aspergillus fumigatus; Lung lesion; Needle aspiration; Mediastinal lymphadenopathy; Serum galactomannan
Introduction
Fine needle aspiration is a type of biopsy procedure. In fine needle aspiration, a thin needle is inserted into an area of abnormal-appearing tissue or body fluid. As with other types of biopsies, the sample collected during fine needle aspiration can help make a diagnosis or rule out conditions such as cancer. In a cavitary lesion, biopsy is obtained from the lesion wall; however, it is usually impossible to get specimens from the pulmonary cavities by either cutting biopsy or fine needle aspiration when they are thin walled.
Case Presentation
A 64-year-old male presented with chills and mild dyspnea on exertion after completing four cycles of chemotherapy for stage IIA adenocarcinoma of the lung. Five months prior to presentation, he underwent left upper lobe lobectomy. He denied cough, chest pain or fever. On examination, he was afebrile with normal vital signs. Chest auscultation revealed normal breath sounds. The rest of the physical examination was unremarkable.
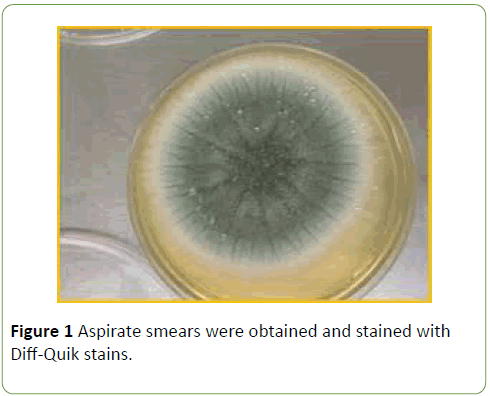
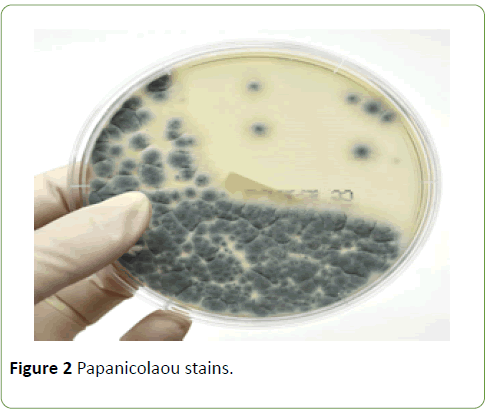
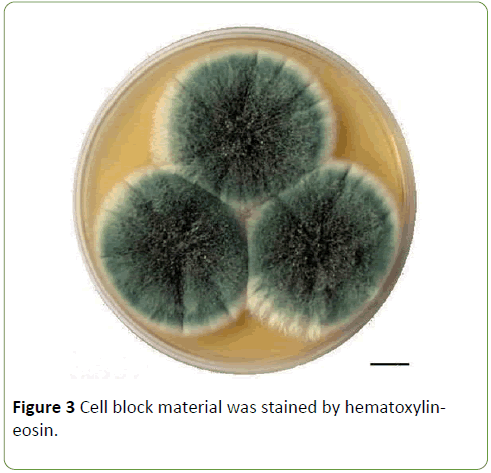
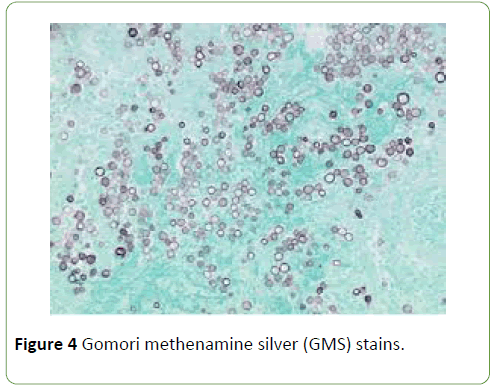
Laboratory tests showed mild anemia but normal values of white blood cell count and platelet count. A chest computed tomography (CT) scan revealed a new 2.2 × 1.8 cm, thickwalled cavitary lesion in the superior aspect of the left lower lobe and mediastinal lymphadenopathy. Serum galactomannan antigen test was negative. A diagnostic CT guided percutaneous left lower lobe fine needle aspirate (FNA) was performed. Using standard procedures, paired aspirate smears were obtained and stained with Diff-Quik stains (Figure 1) and Papanicolaou stains (Figure 2). Cell block material was stained by hematoxylin-eosin (Figure 3) and Gomori methenamine silver (GMS) stains (Figure 4). Cultures for bacteria, fungi and mycobacteria were also obtained.
The imaging findings in our case was concerning for a new primary lung malignancy with mediastinal lymph node involvement, given the patient’s prior history of adenocarcinoma. However cytological examination of lung aspirate revealed numerous fungal conidial and hyphal elements. The smears showed no malignant cells but demonstrated mucin strings and entangled hyphae in a background of inflammatory and necrotic debris (Figure 1). Numerous fungal hyphae were visible on all preparations with no evidence of malignancy.
Fungal culture confirmed the presence of rare growth of Aspergillus fumigatus. The patient was offered treatment with voriconazole for suspected invasive disease but refused treatment due to concerns of adverse effects. Subsequent clinical course and serial chest imaging findings over a period of 6 months revealed progression of primary lung cancer with metastasis. In our patient, the detection of Aspergillus fumigatus on FNAC likely reflects colonization of the lung cavity and not invasive disease.
Discussion
The differential diagnosis of a newly diagnosed cavitary lesion on chest imaging in an immunocompromised host is broad and includes malignancy and a variety of opportunistic infections, non-infective granulomatous disease, and vascular infarcts [1,2]. A pulmonary cavity is defined as a gas-filled lung area in the center of a nodule or area of consolidation and often detected by chest radiography or CT scan [2]. Malignancy is the most frequently etiology of solitary cavitary nodule in the lung parenchyma and may occur at any location and typically are round or irregular in appearance with a wall thickness greater than 24 mm with associated perilesional consolidation [1,3].
Infectious etiology remains an important cause of cavitary lung disease. The microorganisms causing cavitary lesions in the lung may include bacteria (e.g. Streptococcus species, Staphylococcus aureus including methicillin-resistant Staphylococcus aureus, Klebsiella species, anaerobes); Mycobacteria (e.g. Mycobacterium tuberculosis, atypical mycobacteria), fungi (e.g. Aspergillus species); and rarely parasites [1,2]. Aspergillus fumigatus is a ubiquitous hyaline mold which can cause serious and sometimes fatal infections in immunocompromised patients; in this setting, the organism causes disease predominantly in the lungs although dissemination to virtually any organ can occur [4,5]. In patients with altered lung function or individuals with an immunocompromised status, Aspergillus spp. can cause a variety of pathological entities, including allergic bronchopulmonary aspergillosis, aspergilloma (occur in patients with underlying cavitary disease), chronic necrotizing aspergillosis and invasive pulmonary aspergillosis, seen primarily in immunocompromised patients [6].
Conclusion
Fine needle aspiration cytology (FNAC) can be quite helpful in distinguishing malignancy from infection [7]. Fungal elements may be detected using routine stains as in our case. GMS special stain may be performed on cell block material. However, cavitary lung cancer, especially with cartilage tissue in the cavity wall can mimic aspergilloma [8]. The diagnostic utility of fine needle aspiration cytology to detect a wide variety of opportunistic pulmonary infections in an immunocompromised host has been studied. FNAC techniques are safer, cost-effective and provide rapid results [7]. Use of special stains to enhance cytomorphological changes in conjunction with microbiology culture results is critical to identify the specific microorganism.
References
- Ryu JH, Swensen SJ (2003) Cystic and cavitary lung diseases: Focal and diffuse. Mayo Clin Proc 78: 744-752.
- Gadkowski LB, Stout JE (2008) Cavitary pulmonary disease. Clin Microbiol Rev 21: 305-333.
- Chaudhuri MR (1973) Primary pulmonary cavitating carcinomas. Thorax 28: 354-366.
- Patterson TF, Thompson GR, Denning DW, Fishman JA, Hadley S, et al. (2016) Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis 63: e1-e60.
- Chabi ML, Goracci A, Roche N, Paugam A, Lupo AN, et al. (2015) Pulmonary aspergillosis. Diagn Interv Imaging 96: 435-442.
- Franquet, T, Müller NL, Oikonomou, A, Flint JD (2004) Aspergillus infection of the airways: Computed tomography and pathologic findings. J Comput Assist Tomogr 28: 10-16.
- Sharma S, Gupta P, Gupta N, Lal A, Behera D, et al. (2017) Pulmonary infections in immunocompromised patients: the role of image-guided fine needle aspiration cytology. Cytopathology 28: 46-54.
- Taoka T, Shinohara T, Naruse K, Ogushi F (2017) Cavitary lung cancer with cartilage tissues in the wall mimicking aspergilloma. Thorax 72: 383-384.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences