A Parathyroid Adenoma Dorsal of the Esophagus, An Ectopic Localization
Dulfer RR, Hartholt KA and Smit PC
DOI10.21767/2471-8041.100052
Dulfer RR, Hartholt KA* and Smit PC
Department of Surgery, Traumatology, Reinier de Graaf Group, The Netherlands
- *Corresponding Author:
- Hartholt KA
Faculty, Department of Surgery
Traumatology, Reinier de Graaf Group
Reinier de Graafweg 3-11
2625AD, Delft, The Netherlands
Tel: +31 15 260 3060
E-mail: k.hartholt@erasmusmc.nl
Received Date: April 11, 2017; Accepted Date: May 14, 2017; Published Date: May 17, 2017
Citation: Dulfer RR, Hartholt KA, Smit PC. A Parathyroid Adenoma Dorsal of the Esophagus, An Ectopic Localization. Med Case Rep, 3:2. Doi: 10.21767/2471-8041.100052
Abstract
A 65-year-old female was analyzed because of obstipation and hypercalcaemia, which was the result of primary hyperparathyroidism. The parathyroid adenoma was ectopically located. Initial physical examination was performed, followed by subsequent laboratory and ultrasound examination, tc-99m sestamibi scintigraphy and computed tomography. It revealed a parathyroid gland with an ectopic localization dorsally of the esophagus. The ectopic parathyroid adenoma was surgically removed, and her complaints disappeared.
Keywords
Ectopic parathyroid adenoma; Hyperparathyroidism
Introduction
Parathyroid adenomas are benign tumors of the parathyroid gland, which often cause hyperparathyroidism. The parathyroid glands are generally located on behind the thyroid gland in the neck. In general, humans have four pea-sized parathyroid glands. Since less than 0.1% of the inferior parathyroid glands are located ectopically [1]. Our case represents a rare finding. It is important to identify all possible locations of abberant pararthyroid locations in order to aid physicians in future diagnostic dilemma’s regarding hyperparathyroidism.
Case Presentation
A 65-year-old female was admitted to the department of Internal Medicine, because of hypercalcaemia. She presented with obstipation, abdominal pain, and muscle ache, loss of energy, dizziness and joint pain in shoulders, hands, knees, and feet. Her medical history included a uterus myomatosus, uterus prolapse, adnexa extirpation and sterilization, appendectomy, hypertension, tuberculosis and a transient ischemic attack.
Physical examination did not reveal any abnormalities. Laboratory tests showed an increased calcium of 3.60 (2.20-2.65 mmol/L), increased parathyroid hormone (PTH) of 72 (1.6-6.8 pmol/L) and increased vitamin D 1.25 of 430 (43-168 pmol/L).
Due to a suspected primary hyperparathyroidism, additional imaging was performed. No abnormalities were seen on a ultrasound of the neck and (para)thyroid glands. A Tc-99m sestamibi scintigraphy showed no lesions in the neck; however it did reveal a lesion suspected for an ectopical parathyroid adenoma paratracheal on the dorsal left side.
The patient was initially treated for hypercalcaemia with aminopropylidine diphosphonate (APD) infusion and Mimpara. Mimpara is a calcimimetic which activates the calcium-sensing receptor. This inhibits PTH secretion and lowers serum calcium levels. However, due to symptoms of hypocalcaemia the patient stopped using Mimpara after a while. The serum calcium levels normalised, although PTH remained elevated at 73 pmol/L.
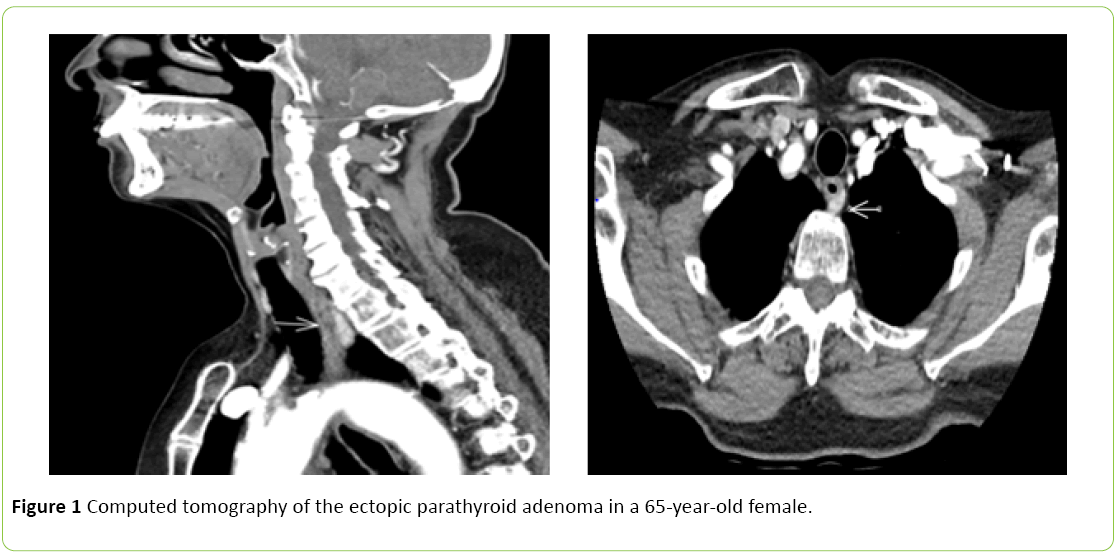
During time, her calcium levels increased slowly, after the Mimpara was stopped. Because she did not want to use medication, she was referred to the surgical outpatient clinic. At 7 months after initial presentation, a CT-scan of her neck was performed to determine the exact location of the suspected ectopic parathyroid adenoma. The CT-scan showed the presence of a sharp defined lesion of 2.0 × 1.1 × 0.5 cm ventral to the vertebral corpus of thoracic vertebra 1 and left dorsal to the oesophagus, corresponding to the lesion on the Tc-99m sestamibi scintigraphy (Figure 1). A resection of the suspected adenoma was planned.
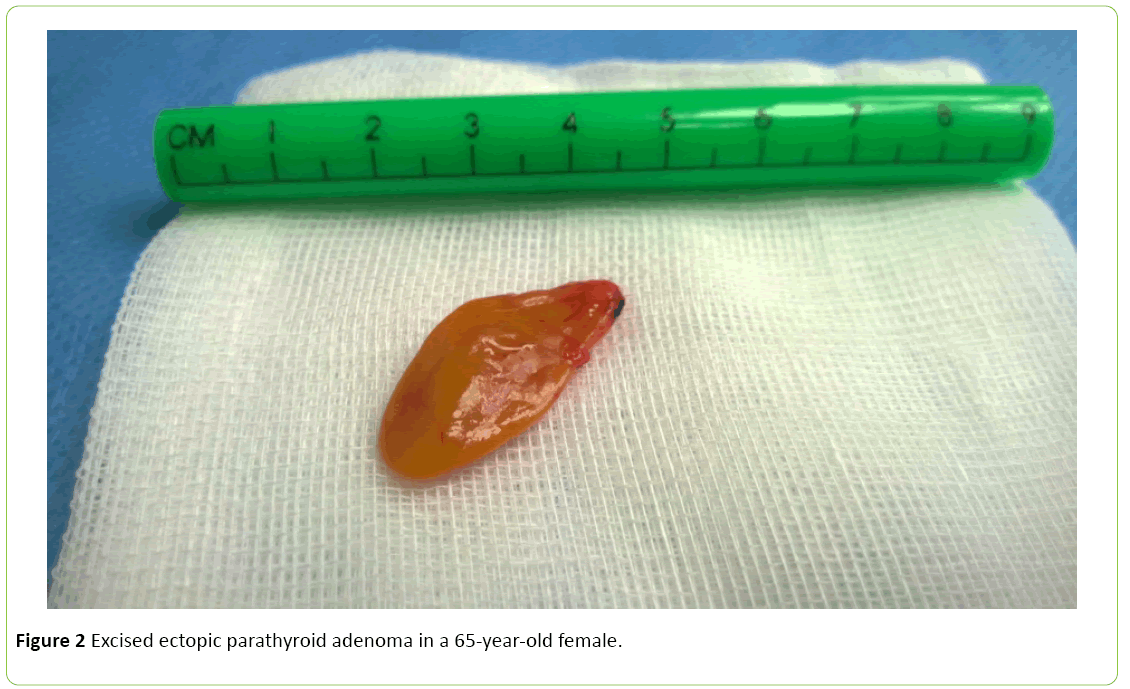
During surgery (a minimal invasive adenectomy) complete excision of the ectopic parathyroid adenoma was achieved without complications. Figure 2 shows the ectopic parathyroid adenoma during surgery.
Differential diagnosis
In this case, the diagnosis was primary hyperparathyroidism due to a parathyroid adenoma with an ectopic localization. Primary hyperparathyroidism can be present in patient with multiple endocrine neoplasia (MEN-syndrome). In case of endocrine tumors in family history, further diagnostics are warranted. In this case, there were no familiar endocrine tumors.
Treatment
Symptomatic hyperparathyroidism (nephrolithiasis, symptomatic hypercalcemia) is always an indication for treatment. In asymptomatic hyperparathyroidism, indications for treatment are listed in the guidelines from the Fourth International Workshop on Asymptomatic Primary Hyperparathyroidism [2-9].
Only definitive care in primary hyperparathyroidism consists of surgical excision of the parathyroid adenoma(s). Medical treatment is reserved for patients who are poor surgical candidates. Hypercalcaemia can be treated with Mimpara. Bisphosphonates can increase bone mineral density.
Outcome and follow-up
Surgical excision of the ectopic parathyroid adenoma was achieved without complications. Histological analysis concluded a parathyroid adenoma with a weight of 0.99 gram.
During follow-up at the outpatient clinic there were no symptoms of hyperparathyroidism. At 2 months after surgery the calcium levels remained normal (2.46 mmol/L) and the PTH level normalised (5.5 pmol/L).
Discussion
In general, the parathyroid glands are located on the thyroid gland in the neck. In 85% of humans, four pea-sized parathyroid glands are present. The parathyroid glands produce PTH which regulates calcium and phosphate homeostasis. In case of PTH overproduction serum calcium levels are increased through enhanced bone resorption, increased intestinal calcium absorption and decreased urinary excretion [1].
As mentioned before, primary hyperparathyroidism is in 90% the cases caused by a solitary parathyroid adenoma [2-5]. The other 10% is caused by multiple adenomas, parathyroid hyperplasia of a very rare parathyroid carcinoma. Since only less than 0.1% of the inferior parathyroid glands are located ectopically, our case presents a rare finding [1].
After diagnosing primary hyperparathyroidism through biochemical evaluation, preoperative parathyroid localization studies are used to localize a parathyroid adenoma. In case of a single adenoma an excision by minimally invasive surgery is the preferred course of treatment. Patients suitable for a minimally invasive surgical approach require concordant localizing studies [6-10]. If imaging is not concordant, exploration with intra-operative PTH measurements is indicated.
The most common cause of persistent hyperparathyroidism is a missed parathyroid adenoma [11]. The most common site of missed adenomas is the tracheal-oesophageal groove in the posterior superior mediastinum (27%). In case of a missing gland it is important to distinguish between superior and inferior glands, which can be established based upon e.g. their migration pattern [12]. Superior glands in general migrate minimally caudally towards the dorsal surface of the thyroid gland. Inferior glands in general migrate caudally and medially and thus can be localized anywhere between the pericardium and jaw [12,13]. Ectopic parathyroid adenomas are predominantly located in the thymus (38%), followed by the retro-oesophageal region (31%) and intrathyroidal (18%) [14].
Postoperative complications after parathyoidectomy are rare. Complications which could occur are among others: operative failure, wound infection, hematoma, postoperative mild or severe hypocalcaemia, recurrent laryngeal nerve injury, and permanent hypoparathyroidism.
Postoperative hypocalcaemia is an important complication, which occurs within the first 24 to 48 hours after surgery. For this reason, calcium and serum PTH should be monitored. Distinction between mild and severe hypocalcaemia can be made postoperative. Hypocalcaemia can be characterized by tetany, seizures, paraesthesia’s, anxiety, depression, hypotension, bradycardia and papilledema.
Mild hypocalcaemia is generally treated through a short period of daily 1500-2000 mg oral calcium suppletion due to calcium carbonate or citrate. Patients with severe hypocalcaemia should be treated with oral and intravenous calcium supplementation. Thereby concomitant hypomagnesemia should be corrected [15].
In this case, the patient did not suffer from hypocalcaemia. In summary, we report a case of an ectopic parathyroid adenoma located dorsal of the oesophagus in a 65-year-old female. Less than 0.1% of the inferior parathyroid glands are located ectopically.
Conclusion and Learning Points
Primary hyperparathyroidism is usually caused by a solitary parathyroid adenoma.
Less than 0.1% of the inferior parathyroid glands are located ectopically.
In case of suspected ectopic parathyroid adenoma additional CT-scanning is advantageous to localize the adenoma and establish anatomical relations.
References
- Zerizer I, Parsaï A, Win Z, Al-Nahhas A (2011) Anatomical and functional localization of ectopic parathyroid adenomas: 6-year institutional experience. Nucl Med Commun 32: 496-502.
- Gooszen HG (2006) Leerboekchirurgie. Uitgever: Houten. Bohn Stafleu van Loghum.
- Chiu NT, Cheng HM, Yao WJ (1995) Tc-99m sestamibi scanning in the preoperative localization of mediastinal parathyroid adenomas. Ann Nucl Med 9: 157-159.
- Tublin ME, Pryma DA, Yim JH, Ogilvie JB, Mountz JM, et al. (2009) Localization of parathyroid adenomas by sonography and technetium tc 99m sestamibi single-photon emission computed tomography before minimally invasive parathyroidectomy: are both studies really needed? J Ultrasound Med 28:183-190.
- Boom RPA, Peterse JL (1986) A patient with a parathyroid carcinoma. Ned TijdschrGeneeskunde 130: 1117-1120.
- Udelsman R (2002) Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 235: 665-670.
- Grant CS, Thompson G, Farley, Van Heerden J (2005) Primary hyperparathyroisodm surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic Experience. Arch Surg 140: 427-428.
- Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, et al. (2009) Reoperation for parathyroid adenoma: A contemporary experience. Surgery 146:1144-1155.
- Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, et al. (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: Summary statement from the Fourth International Workshop. J ClinEndocrinolMetab 99: 3561.
- Hindié E, Mellière D, Perlemuter L, Jeanguillaume C, Galle P (1997) Primary hyperparathyroidism: higher success rate of first surgery after preoperative Tc-99m sestmibi-I-123 subtraction scanning. Radiology 204: 221-228.
- Jaskowiak N, Norton JA, Alexander HR, Doppman JL, Shawker T, et al. (1996) A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg 224: 308.
- Musters L, Van Ginhoven TM, Smit C (2014) Exceptional localisation of an ectopic parathyroid adenoma at the level of the hyoid bone. BMJ Case Rep.
- Bassler T, Wong ET, Brynes RK (1993) Osteitisfibrosacystica simulating metastatic tumour. An almost forgotten relationship. Am J Clin Path 100: 697-700.
- Roy M, Mazeh H, Chen H, Sippel RS (2013) Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg 37: 102-106.
- Perrier ND, Dickson VP, Figueroa AS (2013) Parathyroid exploration for primary hyperparathyroidism (PHPT) – An Up-to-Date.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences