Takatomo Mine, Michiko Fukami, Koichiro Ihara, Hiroyuki Kawamura, Ryutaro Kuriyama and Ryo Date
Takatomo Mine, Michiko Fukami, Koichiro Ihara, Hiroyuki Kawamura, Ryutaro Kuriyama and Ryo
Date
DOI10.21767/2471-8041.100038
Takatomo Mine*, Michiko Fukami, Koichiro Ihara, Hiroyuki Kawamura, Ryutaro Kuriyama and Ryo Date
Department of Orthopaedic Surgery, National Hospital Organization, Kanmon Medical Center, Yamaguchi, Japan
- *Corresponding Author:
- Takatomo Mine
Department of Orthopaedic Surgery, National Hospital Organization, Kanmon Medical Center, 11 Chofu Ushiroda Simonoseki , Yamaguchi 752-8510, Japan
Tel: +81-83-2411199
Fax: +81-83-2411301
E-mail: minet@kanmon-mc2.hosp.go.jp
Received date: December 30, 2016; Accepted date: March 03, 2017; Published date: March 06, 2017
Citation: Mine T, Fukami M, Ihara K, et al. Juvenile Idiopathic Arthritis Simulating Osteochondral Injury of the Knee. Med Case Rep. 2017, 3:1. doi: 10.21767/2471-8041.1000038
Abstract
Timely diagnosis and appropriate aggressive treatment of patients of juvenile idiopathic arthritis (JIA) improve quality of life and outcome. In a reported case of JIA, symptoms started after knee strain occurred while walking. Arthroscopic examination and magnetic resonance imaging was helpful. Treatment with MTX and adalimumab was effective and there was no recurrence for one year.
Keywords
Juvenile idiopathic arthritis; Arthroscopy; Osteochondral injury; Biological DMARDs
Introduction
Juvenile idiopathic arthritis (JIA) is defined as arthritis of unknown etiology. It is the most common rheumatic disease entity in childhood with a prevalence of 0.6-1.9 per 1000 children [1,2]. It is sometimes difficult to differentiate JAI from conditions such as infections, tumors, and reactive arthritis. If arthritis and inflammation of the knee are untreated and progress over the long term, articular destruction can occur. In the patient reported here, symptoms were precipitated by knee strain while walking. The initial diagnosis was osteochondral injury of the lateral tibial plateau. However, a limp associated with bilateral knee pain and swelling subsequently developed without any systemic symptoms.
Case Report
A 15-year-old girl developed pain in her right knee while walking downhill and consulted a physician. MRI revealed osteochondral injury of the lateral tibial plateau, and conservative therapy was recommended. However, her symptoms did not improve and the patient was referred to us seven months later. She complained that she could not go up and down stairs. There was no fever, no other joint pain and no systemic symptoms. Her past history and family history were unremarkable.
At the initial examination, swelling and effusion of the right knee joint were noted, but there was no redness or localized heat. The range of knee motion was normal and there were no signs indicating damage to the menisci or ligaments. Slight swelling of the left knee was also present.
Laboratory tests revealed that Hb was 13.2 g/dl, WBC was 7400, and CRP was 0.42 mg/dl. Rheumatoid factor, ACPA, and anti-nuclear antibodies were negative, while MMP3 was 173.1 μg. The aspirated synovial fluid was yellowish and slightly turbid. Bacterial culture was negative.
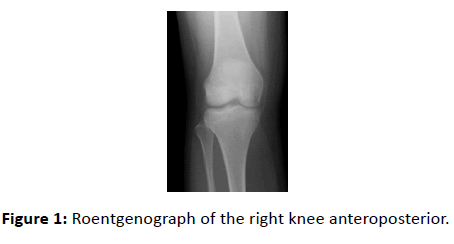
The X-ray film showed a small bone defect of the lateral tibial plateau of the right knee (Figure 1).
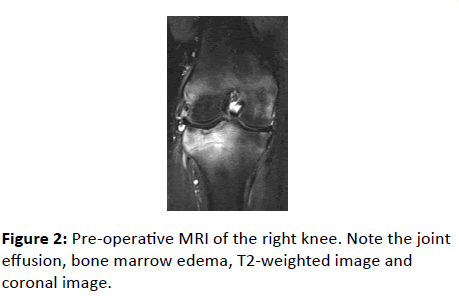
MRI revealed effusion, bone marrow edema and bone erosion of the right knee joint, with no obvious abnormalities of the menisci or articular cartilage (Figure 2).
Arthroscopic examination was conducted under general anesthesia. The menisci and articular cartilage were intact, but synovial hypercellularity was noted.
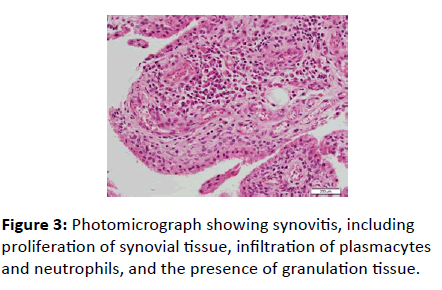
Histological examination revealed signs of synovitis, including proliferation of synovial tissue, infiltration of plasmacytes and neutrophils, and the presence of granulation tissue (Figure 3).
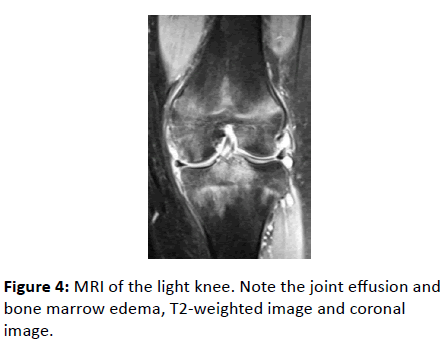
These findings were highly suggestive of juvenile idiopathic arthritis (JIA). Type of JIA might be considered as Oligoarthritis. From 2 weeks after arthroscopy, administration of methotrexate (MTX) was initiated at 10 mg/day, resulting in slight improvement of her right knee symptoms. However, pain and swelling of the left knee appeared. MRI identified joint effusion, bone marrow edema and bone erosion of the left knee joint, with no obvious abnormalities of the menisci or articular cartilage (Figure 4).
MTX was increased to 12 mg/day three months after administration of MTX 10 mg/day, leading to improvement of the left knee symptoms. However, pain and swelling of the right knee persisted. Administration of MTX at a higher dose than 12 mg/day led to adverse effects, so tocilizumab was initiated after assessment of TSPOT and 1, 3-βD-Glucan (BG) assay. CRP and ESR became negative after two months, but her symptoms persisted. Tocilizumab was changed to adalimumab, and her symptoms subsided immediately. Treatment with 12 mg/day MTX and adalimumab was continued and there was no recurrence for one year.
Discussion
Diseases that need to be differentiated from JIA of the knee in children are JRA, infection, neoplasms, reactive arthritis, hemophilia, and pigmented villonodular synovitis. Diagnosis of JIA is based on clinical and laboratory findings. In the present case, symptoms started after knee strain occurred while walking. At first, the patient was considered to have osteochondral injury of lateral tibial plateau. Her symptoms were limited to the knees without any systemic manifestations. Laboratory tests showed elevation of CRP, while rheumatoid factor and anti-cyclic citrullinated peptide antibody were negative. These findings were equivocal.
Several studies have shown that MRI can provide precise quantification of synovitis in children with JIA [3-5]. MRI also reveals a high frequency of bone marrow edema and bone erosions early in the course of this disease. Johnson stated that hypervascular synovium, joint effusion, irregularity of the infrapatellar fat pad, soft tissue swelling, and popliteal lymphadenopathy, all of which can be observed by MRI, are important in the early diagnosis of JIA, emphasizing the need for imaging with gadolinium contrast medium [6]. However, it is difficult to make a definite diagnosis of JIA from MRI alone. Arthroscopic confirmation of the presence of synovitis and the state of the menisci or articular cartilage can assist in the diagnosis. Rydlholm [7] and Gattinara [8] reported that arthroscopic synovectomy is an effective procedure, but articular destruction still tends to progress in some patients. Kvien performed a two-year observational study and concluded that the clinical outcome was more satisfactory in patients who had undergone synovectomy [9]. In the present patient, only limited arthroscopic synovectomy was conducted.
Conclusion
Synovectomy may be more important as a diagnostic procedure, while medical therapy is the mainstay of treatment for JIA. Weekly methotrexate has been established as an effective treatment for polyarticular JIA and biological DMARDs are also efficacious for polyarticular disease. There is a lack of consensus-driven, evidence-based treatment guidelines. In 2015, NHS England released a policy statement, ‘Biologic Therapies for the treatment of Juvenile Idiopathic Arthritis’ [10]. The guideline advised a TNF inhibitor can be started immediately with poor response to MTX. Brunner reported good result for the use of tocilizumab in patients with polyarticular JIA who had not achieved a good response with MTX and a TNF inhibitor [11]. Turnier reported that tocilizumab had an impottant and evolving role in controlling disease activity in patients with JIA [12]. In Japan, biological DMARDs including adalimumab, tocilizumab and abatacept have been approved for JIA. In this case, tocilizumab was not sufficiently effective. Adlimumab improved signs and symptoms. The biological DMARDs should be chosen for reason of effectiveness and safety.
References
- Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369: 768-778.
- Prakken B, Albani S, Martini A (2011) Juvenile idiopathic arthritis. Lancet. 377: 2138-2149.
- Gattinara M, Lomater C, Paresce E, Minola R, Vigano R, et al. (1994) Arthroscopic synovectomy of the knee joint in the treatment of patients with juveniles chronic arthritis. Acta Univ Carol Med 40: 113-115.
- Johnson K, Wittkop B, Haigh F, Ryder C, Gardner-Medwin JM (2002) The early magnetic resonance imaging features of the knee in juvenile idiopathic arthritis. Clin Radiol 57: 466-471.
- Kvien TK, Pahle JA, Hoyeraal HM, Sandstad B (1987) Comparison of synovectomy and no synovectomy in patients with juvenile rheumatoid arthritis. A 24-month controlled study. Scand J Rheumatol 16: 81-91.
- Malattia C, Damasio MB, Magnaguagno F (2008) Magnetic resonance imaging, ultrasonography, and conventional radiography in the assessment of bone erosions in juvenile idiopathic arthritis. Arthritis Rheum 59: 1764-1772.
- Magni-Manzoni S, Malattia C, Lanni S, Ravelli A (2012) Advances and challenges in imaging in juvenile idiopathic arthritis. Nat Rev Rheumatol 8: 329-336.
- Hemke R, Van Veenendaal M, Van den Berg JM, Dolman KM, Van Rossum MA, et al. (2014) One-year followup study on clinical findings and changes in magnetic resonance imaging-based disease activity scores in juvenile idiopathic arthritis. J Rheumatol 41: 119-127.
- Rydholm U, Elborgh R, Ranstam J, Schroder A, SvantessonÃÆãÃâââ¬Ãâââ¬H,ÃÆãÃâââ¬Ãâââ¬et al. (1986) SynovectomyÃÆãÃâââ¬Ãâââ¬ofÃÆãÃâââ¬Ãâââ¬theÃÆãÃâââ¬Ãâââ¬kneeÃÆãÃâââ¬Ãâââ¬inÃÆãÃâââ¬Ãâââ¬juvenileÃÆãÃâââ¬Ãâââ¬chronicÃÆãÃâââ¬Ãâââ¬arthritis.ÃÆãÃâââ¬Ãâââ¬J Bone Joint Surg 67-A: 8-15.
- Entgland N (2015) Interim Clinical Commissioning Policy Statement: Biologic therapies for the treatment of juvenile idiopathic arthritis (JIA).
- Brunner HI, Ruperto N, Zuber Z, Keane C, Harari O, et al. (2015) Efficacy and safety of tocilizmab in patients with polyarticular-course in juvenile idiopathic arthritis: Results from a phase-3, randomized, double-blind withdrawal trial. Ann Rheum Dis 74: 1110-1117.
- Turnier JL, Brunner HI (2016) Tocilizumab for treatment juvenile idiopathic arthritis. Expert Opin Biol Ther 16: 559-566.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences