Outcome of A Non Healing Pancreatico-Cutaneous Fistula, Treated with Local Tetracycline Instillation – A Case Report
Kumarasinghe NR, Ileperuma SK, Dassanayake BK, Pinto V and Galketiya KB
DOI10.21767/2471-8041.1000031
1Department of Surgery, Faculty of Medicine, University of Peradeniya, Sri Lanka
2Department of Anesthesiology, Faculty of Medicine, University of Peradeniya, Sri Lanka
- *Corresponding Author:
- Kumarasinghe NR
Department of Surgery, Faculty of Medicine, University of Peradeniya, Sri Lanka
Tel: +94 718446990
E-mail: navam_k2000@yahoo.com
Received date: May 28, 2016; Accepted date: September 27, 2016; Published date: September 30, 2016
Citation: Kumarasinghe NR, Ileperuma SK, Dassanayake BK, et al. Outcome of A Non Healing Pancreatico-Cutaneous Fistula, Treated with Local Tetracycline Instillation – A Case Report. Med Case Rep. 2016, 2:3. doi: 10.21767/2471-8041.1000006
Abstract
A male 39-years of age presented with generalized abdominal pain of 2 days, associated with fever, anorexia and vomiting. Examination findings were consistent with peritonitis Biochemical indices had neutrophillic leucocytosis and high C-reactive protein. X-ray abdomen has distended bowel loops but no gas under diaphragm. Ultrasonography had limited value due to distended bowel loops.
Introduction
Pancreatic fistulas continue to be of significant morbidity, causing longer hospital stay and incur a high cost. It commonly results as a complication of acute pancreatitis, pancreatic surgery and splenectomy [1].
The reported incidence of pancreatic fistula following pancreatico-duodenectomy is 6-14% [2,3]. However, after distal pancreatectomy, it is much lower (0.5%) [4]. Transection at the pancreatic body, splenectomy, failure to close pancreatic duct and non-use of peri-operative somatostatin agonist (Octreotide) are thought to be risks for fistulation following distal pancreatectomy [5-7].
In the absence of sepsis, a majority of pancreatic fistulas are likely to heal with conservative management alone [8,9]. This includes parenteral nutrition (PN) while resting the bowel, drainage of collections, antibiotics and use of octeotride. However clinical trials have shown conflicting evidence regarding the use of octreotide in managing pancreatic fistulas [10-12]. Those which show resistant to healing will need interventions [1]. Surgical techniques for the treatment of intractable pancreatic fistula include percutaneous transfistulous pancreatic duct drainage (PTPD), percutaneous transfistulous pancreatojejunostomy (PTPJ), and percutaneous transfistulous pancreatic duct embolization (PTPE) [1,2].
This report is based on a non-operative therapeutic strategy, in a young male who developed a cutaneous pancreatic fistula following open drainage of a collection of pus in the pancreatic bed and splenic region.
Case Report
A male 39-years of age presented with generalized abdominal pain of 2 days, associated with fever, anorexia and vomiting. Examination findings were consistent with peritonitis. Biochemical indices had neutrophillic leukocytosis and high C-reactive protein. X-ray abdomen has distended bowel loops but no gas under diaphragm. Ultrasonography had limited value due to distended bowel loops.
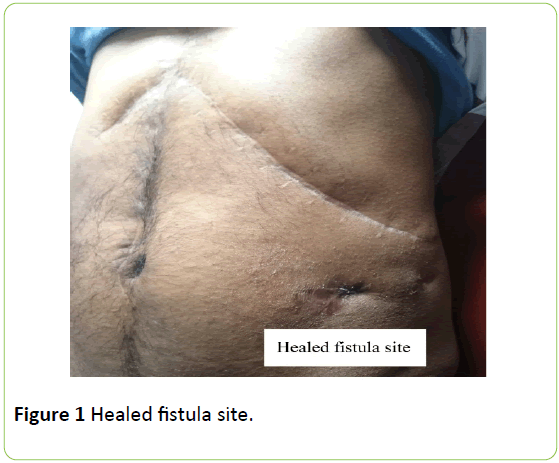
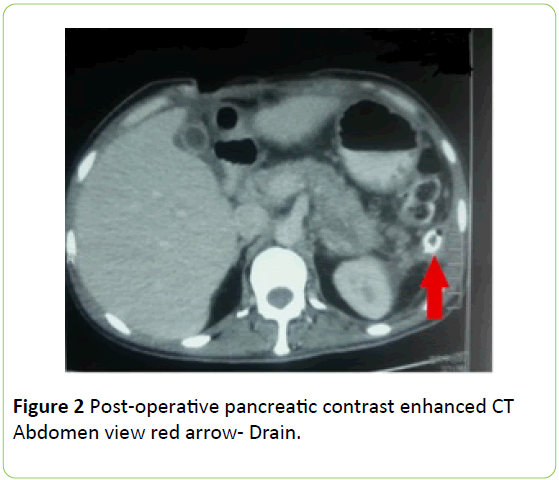
Emergency laparotomy was undertaken. A retroperitoneal pus collection was noted in the left hypochondrium. It was involving the region of the body and tail of pancreas and the spleen. The pus was drained and the spleen which showed features of necrosis was removed. Following thorough peritoneal lavage a drain was placed in the left hypochondrium (Figure 1).
Post operatively signs of sepsis gradually subsided but a continuous drain of thick material was present through the drain. A daily volume of 50-150 ml. persisted. Drain fluid was positive for amylase and drain culture revealed coliforms.
Decisions on managing this pancreatic fistula was a challenge because though various options are mentioned in literature none was very successful and surgery would have been a daunting task in an abdomen with gross adhesions and in a patient who was in a catabolic state. There was also no clear indication for endoscopic retrograde cholangiopancreaticography (ERCP) in post-operative imaging.
Hence we opted for non-operative strategies initially. He was commenced on parenteral nutrition with bowel rest. A Somatostain agonist was added to reduce pancreatic secretions. Drain culture sensitive parenteral antibiotics were started. This trial period was about 2 weeks and little improvement in fistula output was seen and decline in patients’ nutritional state was a concern. Hence we commenced on enteral feeding which helped his general condition improve but not the fistula.
We then resorted to an option of fibrosing the fistula tract. About 6-10 Tetracycline tablets were made in to a powdered solution with isotonic saline and was injected in to the drain. It was noticed that the daily drain volume markedly reduced. Subsequently, following two more tetracycline instillations through the drain on day 03 and day 05 from the first instillation, the fistula output completely ceased (Figure 2).
Discussion
Pancreatic fistulas have been a major concern following surgical intervention of pancreas because of its significant morbidity, longer postoperative recovery and high cost incurred to health institutions. Case series have shown a 6-14% incidence of developing fistulas from pancreaticoenteric anastomosis following pancreatico-duodenectomy [2,3]. However pancreatic leaks which form after distal pancreatectomy and various ennucleation procedures are categorized as pancreatic occlusion failures (POF) [2] and have the low incidence of about 5% amongst specialized centers [4]. These act in a more benign manner and have less morbidity, due to the absence of enzyme acting on pancreatico-enteric anastomosis.
Little is known about risk factors in fistula formation following distal pancreatectomy. BMI >25 kg/m2, transection at the pancreatic body, pancreatic necrosis, operative trauma to pancreatic tail during splenectomy, nephrectomy and splenic flexure mobilization, absence of pancreatic duct ligation and non-use of preoperative somatostatin agonist are several of the implicated factors [6,7].
In this patient presence of pus around the pancreatic tail and spleen, difficulty in identifying clear tissue planes with possible iatrogenic pancreatic injury and failure to close the resected part are risk factors which may have contributed to fistula formation.
Studies have shown that more about 90% patients with distal pancreatic fistulas are managed successfully with nonoperative measures and they seldom require early surgical intervention [13]. In addition, reopening in to a laparatomized abdomen with purulent infection was a challenge because of the fragile adhesions and difficulty in identifying anatomy with possibility of iatrogenic injury. Hence non operative therapeutic measures were implemented.
The main consequences in gastrointestinal fistulas with high outputs are associated with electrolyte imbalances and nutritional deficiencies. Patients are affected by anorexia, poor oral tolerance and malabsorption from gut. Hence initial conservative measures include resting the bowel (nil per oral), giving adequate hydration and correction of electrolytes. However, there is a place for oral feeding with surgically placed naso-jejunal tubes or feeding jejunostomy, bypassing the fistula origin and if the patient tolerates [1]. On the contrary, prolong fasting will need reinforcement with parenteral nutrition support [8,9]. These measures were adopted on this patient, with very limited success in controlling the fistula.
Those which are resistant to heal will need interventions [1]. Surgical techniques for the treatment of intractable pancreatic fistula include percutaneous transfistulous pancreatic duct drainage (PTPD), percutaneous transfistulous pancreatojejunostomy (PTPJ), and percutaneous transfistulous pancreatic duct embolization (PTPE) [1,2]. Peripancreatic collections are amendable for drainage by intervention radiology or surgically. The latter may involve a complete pancreatectomy but this adds a significant mortality to patients [3].
Endoscopic therapy with endoscopic retrograde cholangiopancreaticography (ERCP) has shown benefit. Transpapillary sphincterotomy and stent placement for obstructed pancreatic ducts have improved healing time in some studies but controversies do exist regarding its effectiveness [14-18].
Octeotride is a peptide with similar amino acid sequence to somatostatin. It reduces gastrointestinal exocrine and endocrine secretions. Randomized control studies have shown conflicting evidence regarding its use for reducing the incidence of developing pancreatic fistulas [10-12]. Much of the promising results were seen in high risk patients.
The agent used to heal this fistulous tract is Tetracycline, derived and chemically modified from Actinomycetes [14]. Apart from been an antimicrobial agent, Tetracycline has sclerosing properties and stimulating fibrosis. It was found to be effective in healing postoperative chylous fistulas and broncho-cutaeneous fistulas. Studies have evaluated its ability to heal malignant pleural effusions and suggest the ability of tetracycline to interfere in mesothelial cell repair, induce fibroblast enhancing growth factor secretion and inhibit metalloprotinases as contributory factors [19,20].
Giving consideration to these facts we instilled powdered tetracycline tablets, dissolved in normal saline through the drain tube. A remarkable reduction in drain output was noted and by the 3rd local tetracycline instillation the fistula completely ceased to drain. Hence sclerosing properties of tetracycline need consideration as an effective mode in the treatment of pancreatic fistulas.
References
- Jeffrey AB, Jeffrey MH (2013). Management of pancreatic fistulas. Surg Clin N Am 93 611-617.
- Callery MP, Pratt WB, Vollmer CM, (2009) “Prevention and management of pancreatic fistula,” Journal of Gastrointestinal Surgery,.vol. 13, no. 1, pp. 163–173
- Schmidt CM, Powell ES, Yiannoutsos CT, Thomas JH, Eric AW et al.,(2004)“Pancreaticoduodenectomy: a 20-year experience in 516 patients,” Archives of Surgery, .vol. 139, no. 7, pp. 718–727
- K. D. Lillemoe, S. Kaushal, J. L. Cameron, T. A. Sohn, H. A. Pitt, and C. J. Yeo, “Distal pancreatectomy: indications and outcomes in 235 patients,” Annals of Surgery, (1999) vol. 229, no. 5, pp. 693–700
- Yang YM, Tian XD, Zhuang Y, et al. Risk factors of pancreatic leakage after pancreaticoduodenectomy. World J Gastroenterol 2005;11(16):2456–61.
- Sledzianowski JF, Duffas JP, Muscari F, Suc B, Fourtanier F, (2005) “Risk factors for mortality and intra-abdominal morbidity after distal pancreatectomy,” Surgery, 137: 180–185,.
- Pannegeon V, Pessaux P, Sauvanet A, Vullierme MP, Kianmanesh R, Belghiti J, “Pancreatic fistula after distal pancreatectomy: predictive risk factors and value of conservative treatment,” Archives of Surgery, (2006)vol. 141, no. 11, pp. 1071–1076
- Kazanjian KK, Hines OJ, Eibl G, (2005) “Management of pancreatic fistulas after pancreaticoduodenectomy: results in 437 consecutive patients,” Archives of Surgery., 140: 849–855
- Munoz-Bongrand N, Sauvanet A, A. Denys, A. Sibert, V. Vilgrain, and J. Belghiti, “Conservative management of pancreatic fistula after pancreaticoduodenectomy with pancreaticogastrostomy,” Journal of the American College of Surgeons, vol. (2004) 199, no. 2, pp. 198–203
- Yeo CJ, Cameron JL, Lillemoe KD, Sauter PK, Coleman J et al., (2000) “Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? Results of a prospective randomized placebo-controlled trial,” Annals of Surgery, 232:419–429
- Shan YS, Sy ED, Lin PW, (2003) “Role of somatostatin in the prevention of pancreatic stump-related morbidity following elective pancreaticoduodenectomy in high-risk patients and elimination of surgeon-related factors: prospective, randomized, controlled trial,” World Journal of Surgery, vol. 27, no. 6, pp. 709–714.
- Norman Oneil Machado, (2012) “Pancreatic Fistula after Pancreatectomy: Definitions, Risk Factors, Preventive Measures, and Management—Review,” International Journal of Surgical Oncology, 2012: 10
- Pratt W, Maithel SK, Vanounou T, Callery MP, Vollmer CM, (2006) “Postoperative pancreatic fistulas are not equivalent after proximal, distal, and central pancreatectomy,” Journal of Gastrointestinal Surgery, 10: 1264–1279
- Lloyd Hillyard Conover." American Men & Women of Science: A Biographical Directory of Today's Leaders in Physical, Biological, and Related Sciences. Detroit: Gale, 2008. Gale Biography In Context. Web. 19 Nov. 2011.
- Martin WR, Siefkin AD, Allen R, Chest. (1991) Closure of a bronchopleural fistula with bronchoscopic instillation of tetracycline. 99:1040-42.
- Sauter. BC. (1988) Cytostatic activity of oxidized tetracycline in vitro. Relevance for the treatment of malignant effusions. J. Cancer, 57: 514–515
- Pleurodesis VB, Antony KJ, Rothfuss SW, Codbcv JA, Sparks JW, et al., (1992) Mechanism of tetracycline-hydrochloride-induced. Rev. Respir. Dis., 146: 1009–1013.
- A.N. Hurewitz, C. Liang, P. Mancuso, S. Zucker. (1993) Tetracycline and doxycycline inhibit pleural fluid metalloproteinases. Chest. 103:1113–1117
- Goasguen N, (2009) Endoscopic management of pancreatic fistula after distal pancreatectomy and enucleation. Am J Surg. 197:715–720.
- Grobmyer SR, (2009) Pancreatic stent placement is associated with resolution of refractory grade C pancreatic fistula after left-sided pancreatectomy. Am Surg. 75:654–657.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences