Microskin Grafting for Vitiligo of the Auricle
Devendra K Gupta and Shruti Devendra
Devendra K Gupta* and Shruti Devendra
Department of Plastic Surgery, Devendra Hospital and Yuva Cosmetic Clinic, Bareilly, Uttar Pradesh, India
- Corresponding Author:
- Devendra Kumar Gupta
Devendra Hospital and Yuva Cosmetic Clinic, 55 Prabhat Nagar, Bareilly-243122 Uttar Pradesh, India.
Tel: +919359103564
E-mail: dr.dkgupt@gmail.com
Received date: October 25, 2015; Accepted date: December 04, 2015; Published date: December 11, 2015
Citation: Gupta DK, Devendra S. Microskin Grafting for Vitiligo of the Auricle. Med Case Rep. 2015, 2:2.
Abstract
The various curves, depressions and elevations of the auricle make it challenging to treat, as dermabrasion and retention of the graft is difficult. The purpose of this paper is to prove the usefulness, simplicity and the cost-effectiveness of microskin grafting in treating the vitiligo of the auricle successfully. In all the six patients, the microskin grafting for vitiligo of the auricle was successful. The near total pigmentation was achieved within 3-6 months. The donor area deformities were hardly noticed in post auricular areas as the harvested graft was uniformly thin. No post-operative photochemotherapy was given. The ambulation was not a problem as the graft was harvested from the post-auricular area, with the exception of one patient, in whose case the graft was taken from the thigh. The microskin grafting represents promising, simple and cost-effective therapy for vitiligo of difficult-to-treat site such as the auricle.
Keywords
Vitiligopinna; Leucodermaconcha; Surgical management; Periauricular; Melanocyte
Introduction
Vitiligo is an acquired discoloration of skin and mucous membrane of great cosmetic importance affecting 1-4% of the world's population. The most common variety observed was vitiligo vulgaris (66%), followed by acro-facial (11%), mucosal (10%), focal (7%), segmental (4%), and universalis (2%). Seventynine percent of patients had more than 10% body surface area involvement, 80% had involvement of exposed areas, and 67% had an actively progressive disease. [1] The surgical management of the vitiligo of the auricle is a challenging task due to its uneven surfaces which are difficult to reach for surgical tools. The authors have noticed that most of the patients of vitiligo of the concha of the auricle are of vitiligo vulgaris variety and very few of focal or segmental type. Vitiligo vulgaris is a type of non-segmental, bilateral and usually symmetrical vitiligo while focal vitiligo is a localized form of vitiligo. Segmental type is usually localized to one dermatome and of unilateral variety. On searching the English medical literature, the authors could not find any article related to management of vitiligo of the Concha and auricle. The authors have used here the microskin grafting technique to repigment these areas with promising results in a very simple and cost-effective manner.
Microskin grafting is a tissue grafting technique. For this, we need a small piece of thin split-thickness skin graft (STSG-T) or ultrathin split-thickness skin graft (STSG-UT). The authors prefer to harvest a small graft from the post-auricular area for the surgical management of vitiligo of the Concha. The harvesting of the graft from other hidden areas like gluteal fold, gluteal region or thigh may lead to hindering the patients’ movements and so, are preferably avoided by the authors.
Materials and Methods
For this study, we selected six cases of stable vitiligo of the auricle aging between 21-29 years. The following equipments were used: authors’ self-designed drag-dermatome for harvesting a thin graft from the post auricular area, fine sharp scissors for preparing microskin grafts (MSGs), finely woven muslin cloth tulle Gras, Jeweler’s forceps for spreading of the MSGs and unique end brushes (stem mounted brushes) for the dermabrasion of the concha and various grooves of the auricle. The microskin grafting was performed under the combination of the regional neuronal blocks with mild sedation.
Surgical technique
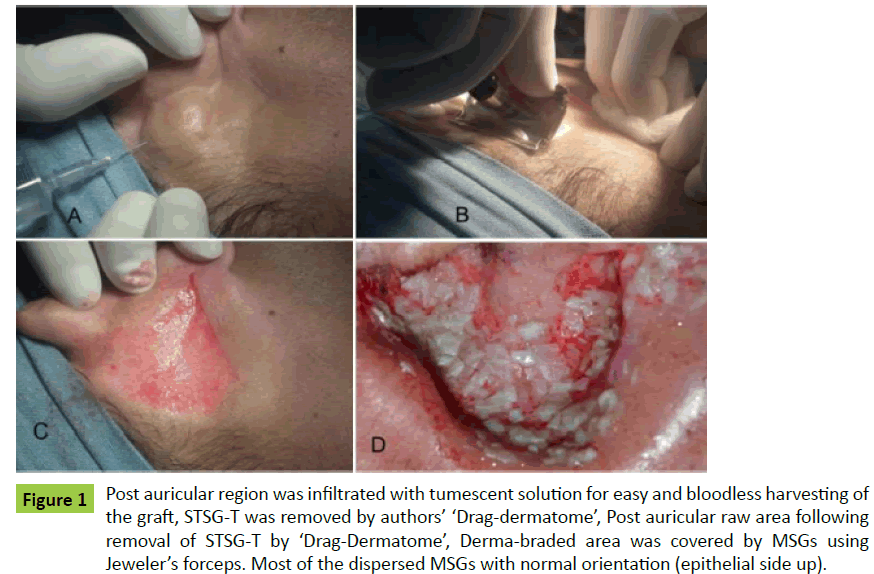
All the patients were operated under mild sedation and regional neuronal blocks. The superficial cervical plexus block was given by inserting the needle at the midpoint of the posterior border of the Sternocleidomastoid muscle. About 7-10 ml of the local anaesthetic solution (half of the 2% lidocaine with adrenaline and half 0.5% Bupivacaine) was injected at this site. This block anaesthetized the lower two-third of pinna. The concha is supplied by the auricular branch of the Vagus nerve, which was blocked by injecting about 2 ml of the local anaesthetic solution in the post-auricular sulcus underneath the Concha. The upper one-third of the pinna is supplied by the auriculo-temporal nerve, which was blocked by injecting 2-3 ml local anaesthetic solution just in front of the tragus. The post-auricular region, which was already anaesthetized by superficial cervical plexus block, was further infiltrated by tumescent solution to minimize bleeding and for easy harvesting of the graft (Figure 1A). The harvesting of the thin split-thickness skin graft (STSG-T) was done from the nonvitiliginous post auricular area by the authors’ drag-dermatome (Figure 1B). The powered dermatome can also be used, but they are too large to be used conveniently and efficiently in this small limited area. The graft was harvested from the thigh in case of bilateral vitiligo of the auricle. The skin graft was put in a small amount of normal-saline for preparation of the MSGs. Small sharp scissors were used to cut the thin sheet of skin graft into tiny particles, (0.2 mm -1 mm) the so-called MSGs. The external auditory meatus was plugged to avoid any debris entering into the auditory canal during dermabrasion. The dermabrasion of all the vitiliginous areas of the auricle was done using special end brushes (stem mounted brushes) (Figure 2B). The dermabrasion was done carefully to peel out the epidermal layer of the skin. Deep abrasions in the skin should be avoided. The MSGs were spread out on all dermabraded areas of the pinna with the help of Jeweler’s forceps. On close observation, it was found that most of the dispersed MSGs were with epithelial side up (Figure 1D). For a rapid pigmentation, we kept the donor to recipient expansion ratio 1:2-1:3. The implanted MSGs were covered with finely woven muslin tulle gras; saline-soaked cotton and at last dry gauze pieces.
Figure 1: Post auricular region was infiltrated with tumescent solution for easy and bloodless harvesting of the graft, STSG-T was removed by authors’ ‘Drag-dermatome’, Post auricular raw area following removal of STSG-T by ‘Drag-Dermatome’, Derma-braded area was covered by MSGs using Jeweler’s forceps. Most of the dispersed MSGs with normal orientation (epithelial side up).
The bandage of the pinna was opened on the eighth day, and it was found that all the dermabraded areas were epithelized in all the patients. The post-auricular donor area healed up in all the patients in 10-12 days. Both the donor and recipient areas were lubricated with coconut oil or any bland moisturizer on a daily basis. Early pigmentation was seen on fifteenth day onward. Complete pigmentation was observed in all the patients in 3-4 months. The initial observation showed a white halo around the external auditory meatus. The most probable reason might be the lack of the dermabrasion of the meatal margin. The dermabrasion at the meatal margin was avoided to keep aside any remote possibility of accidental injury to the ear drum. This white halo at the meatal margin was hardly noticeable as it remained hidden from view. The cobblestone effect was seen in one patient due to the use of little thicker MSGs. This cobblestone effect disappeared by the end of 3 months.
Case Presentations
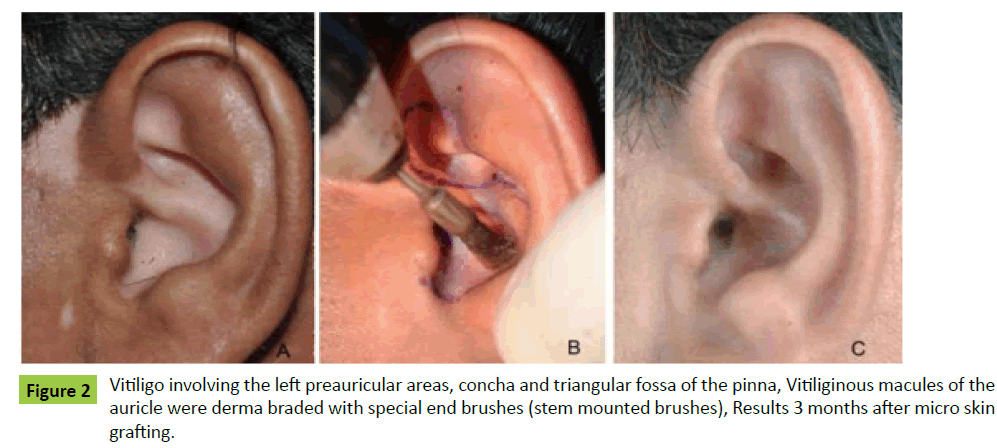
Case 1: A 29-year-old male patient of stable but refractory vitiligo of left ear and the pre-auricular area was presented to us for surgical management (Figure 2A). Under regional anaesthesia, the vitiliginous areas were dermabraded with end brushes (Figure 2B). The most of MSGs dispersed with Jeweler’s forceps were epithelial side up. Near total pigmentation was achieved within three months (Figure 2C).
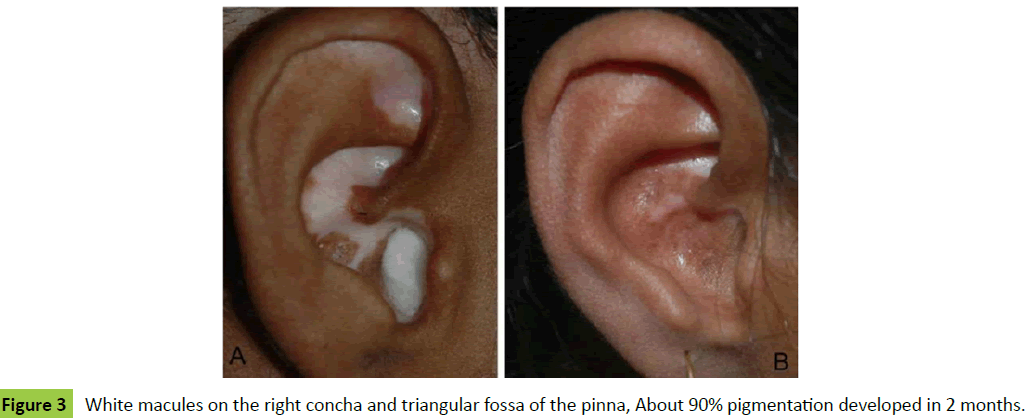
Case 2: A 22-year-old lady was presented to us as a case of vitiligo of her right auricle involving concha and triangular fossa (Figure 3A). Microskin grafting was performed for the management of this refractory vitiligo. The results were obtained at two months (Figure 3B). A few skipped areas could be seen at this early stage.
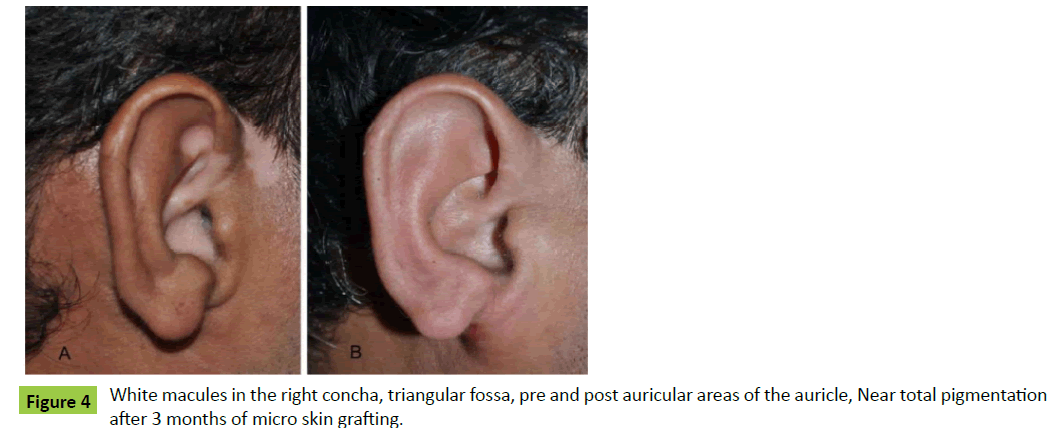
Case 3: A 25-year-old male patient was presented to us for the management of white macules of his right auricle. There were also white macules in pre and post auricular areas (Figure 4A). Microskin grafting was done, and the near normal results were obtained within three months (Figure 4B).
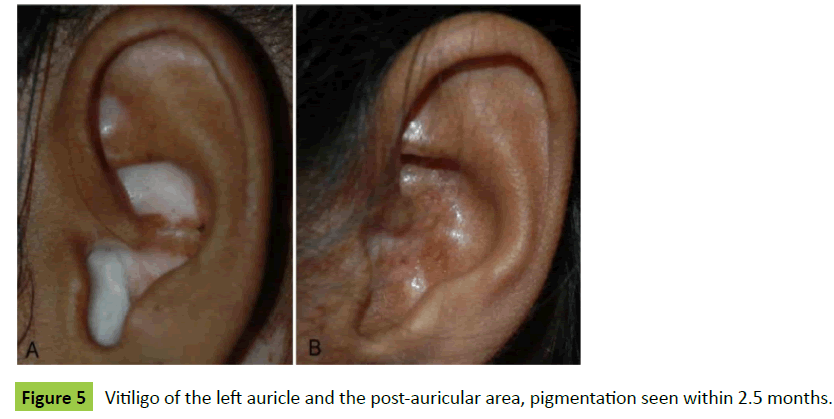
Case 4: A 24-year-old lady was presented to us as a case of vitiligo of left auricle and left-post-auricular area (Figure 5A). The thin skin graft was harvested from her left post auricular area and converted into MSGs. Microskin grafting was done, and the results were seen within two and half months (Figure 5B).
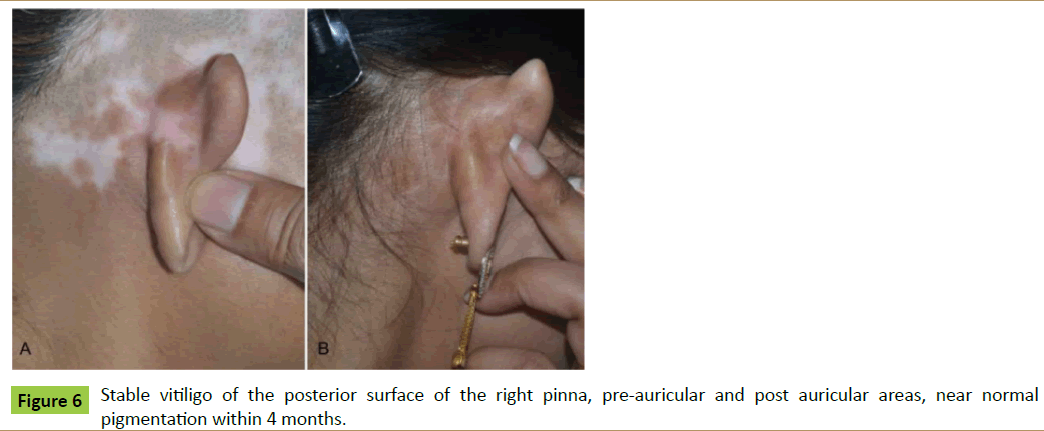
Case 5: A 21-year-old lady was presented to us as a case of stable vitiligo of right temple region and posterior aspect of the pinna (Figure 6A). Microskin grafting was done in the vitiliginous areas. Near total pigmentation was achieved in 6 months (Figure 6B).
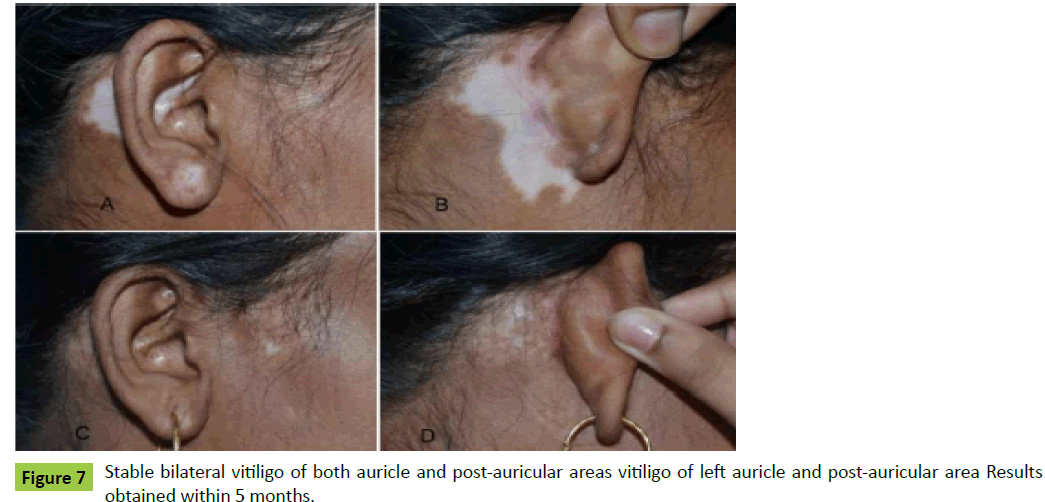
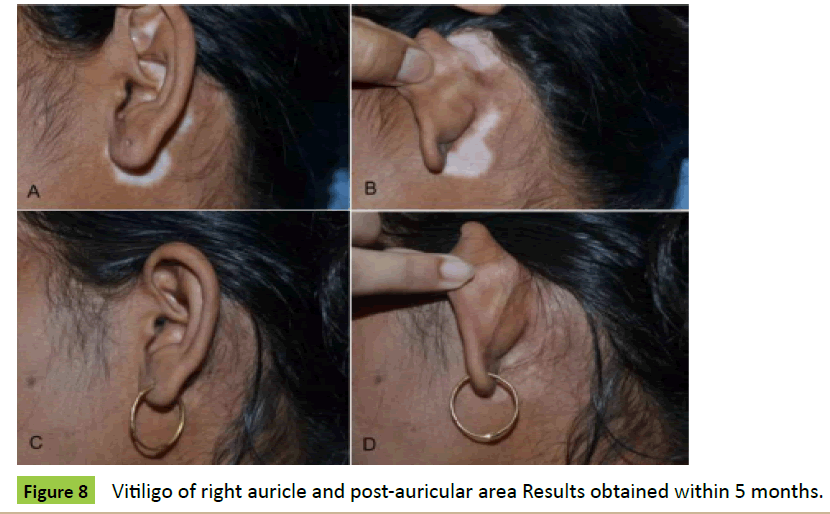
Case 6: A 25-year-old lady was presented to us as a case of stable bilateral vitiligo of both auricle and post-auricular areas (Figures 7A, 7B, 8A and 8B). The ultra-thin skin graft was harvested from her right thigh and converted into MSGs. Microskin grafting was done, and the results were obtained within 5 months (Figures 7C, 7D, 8C and 8D).
Discussion
Tissue-grafting methods, such as minigrafting and blister grafting, are useful to treat small and medium-sized lesions [2,3]. Larger areas can be treated by split-thickness graft [4]. Extensive areas can be treated with the development of cultured [5] and non-cultured [6] cellular transplantations. Various procedures were performed using tiny particles of the thin split-thickness skin graft (STSG-T) for the repigmentation of the stable vitiligo patients. Different authors have given different names to these skin particles such as seed graft [7], smash graft [8], flip-top graft [9], needling micrograft [10], and microskin graft [11]. All the authors have shown good results using skin particles of thin splitthickness skin for the repigmentation of vitiligo. The microskin grafting technique is basically a combination of the procedures, which include harvesting of thin skin-graft, making MSGs quickly for extensive vitiliginous areas, and finally spraying these MSGs on the large vitiliginous areas by using a special spray pump [11]. The surgical management of the vitiligo of the auricle is a little different than other parts of the body. The auricle has different curves, depressions and elevations. The conventional motordriver rotatory wheel wire-brush or diamond fraise is difficult to use for removal of the epidermis from the concha, scapha, etc. The sheet graft, mini punch graft (MPG) or blister graft is difficult to spread for complete ‘take’. The ‘stem mounted brush’ is an ideal tool to remove the epidermis gently from the various curves of the pinna. The MSGs dispersion using jeweler’s forceps and MSGs ‘take’ is not a problem on the auricle. The results with microskin grafting technique are consistently reliable in repigmentation of the vitiliginous areas of the pinna. The microskin grafting technique is a type of tissue grafting technique which is simple, easy and cost-effective, and gives near total normal pigmentation in stable vitiligo of the auricle (Figure 7).
Conclusion
All the six cases of vitiligo of auricle were managed by microskin grafting successfully with a near total pigmentation. The stem mounted brush easily removes epidermis from the intricate regions such as the concha, scapha and other curves of the auricle that are difficult to remove using conventional motordriven wheel burr. The microskin grafting technique is useful, simple, easy-to-learn and execute and also cost-effective for the management of stable vitiligo of the auricle without any noticeable side-effects (Figure 8).
Acknowledgment
No sources of funding were used to prepare this article. The author has no conflicts of interest that are directly relevant to the content of this article.
Ethical standards
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
References
- Mutalik S, Ginzburg A (2000) Surgical management of stable vitiligo: a review with personal experience. DermatolSurg26:248-254.
- Falabella R (2005)Surgical approaches for stable vitiligo. DermatolSurg31: 1277-1284.
- Kahn M, CohenJ (1998) Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. DermatolSurg24: 365-367.
- Olsson M, Juhlin L (1995) Transplantation of melanocytes in vitiligo. Br J Dermatol 91: 587-591.
- MulekarV (2005) Long-term follow-up study of 142 patients with vitiligo vulgaris treated by autologous, non-cultured melanocyte-keratinocyte cell transplantation. Int J Dermatol44: 841-845.
- Katsuhiko T, Atsushi O, Reiko K (2002) Approaches to repigmentation of vitiligo skin: new treatment with ultrasonic abrasion, seed-grafting and psoralen plus ultraviolet A therapy. Pigment Cell Res 15:331-334.
- Krishnan A, Kar S (2012) Smashed skin grafting or smash grafting - a novel method of vitiligo surgery. Int J Dermatol51:1242-1247.
- Sharma S, Garg V (2013) Comparative study of flip-top transplantation and punch grafting in stable vitiligo. DermatolSurg39:1376-1384.
- Sharquie K, NoaimiA, Al-MudarisA (2013) Melanocytes transplantation in patients with vitiligo using needling micrografting technique. J Drugs Dermatol 12:e74-e78.
- Gupta DK (2009) Microskingrafting for vitiligo(1stedn) Springer. London.
- Gupta D, Devendra S (2015)Microskin Grafting for stable vitiligo of the penis and vulva: near total uniform pigmentation. J Cutan Med Surg19:477-483.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences