Infectious Keratitis due to Roseomonas gilardii
Malheiro L, Neves MM, Gomes M and Oliveira L
Malheiro L1*, Neves MM1,2, Gomes M1,2 and Oliveira L1,2
1Department of Ophthalmology, Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, Portugal
2Corneal Unit, Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, Portugal
- *Corresponding Author:
- Malheiro L
Department of Ophthalmology, Hospital de Santo António, Centro Hospitalar Universitário do Porto, 4099-001, Porto, Portugal
Tel: +351918558414
E-mail: luisamalheiro90@gmail.com
Received date: March 08, 2019; Accepted date: April 12, 2019; Published date: April 16, 2019
Citation: Malheiro L, Neves MM, Gomes M, Oliveira L (2019) Infectious Keratitis due to Roseomonas gilardii . Med Case Rep Vol.5 No.2:93.
Abstract
Background: Infectious keratitis is a common ocular pathology and can be caused by a great variety of microorganisms. However, keratitis due to Roseomonas species is an extremely uncommon condition with only two previously reported cases in the literature.
Case presentation: A 70-year-old diabetic male was referenced to ophthalmological emergency due to a corneal ulcer refractory to the treatment with topical moxifloxacin, clotrimazole, prednisolone acetate and oral valacyclovir hydrochloride. The patient had complaints of photosensitivity, pain and blurred vision for 4 weeks. Best corrected visual acuity of the eye was 20/100. Corneal scrapings, collected in the emergency, revealed to be positive for a gram-negative bacillus, producing a pink-pigmented raised colony that was identified, by day 8, as Roseomonas gilardii . Considering the result, the patient immediately started target treatment with topical moxifloxacin and tobramycin. Six days later, there were no signs of active infection. The patient achieved a visual acuity of 20/25.
Conclusion: The course of Roseomonas infection can be insidious and may result in misdiagnosis and delayed target treatment. Corneal scrapers should be done promptly in corneal ulcers refractory to the treatment. It is important to pursue final identification of this pathogen because of its susceptibilities to antibiotics.
Keywords
Case report; Infectious keratitis; Roseomonas gilardii ; Corneal scrapings; Target therapy
Introduction
Infectious keratitis is an important cause of blindness worldwide. A great diversity of pathogens can be responsible for infectious keratitis, however, those related to Roseomonas species have been rarely reported in the literature. This paper aims to report a clinical case of an infectious corneal ulcer in a diabetic male patient caused by Roseomonas gilardii , detailing its management and outcome. Considering the rarity of Roseomonas as a cause for infectious keratitis, we attempt to describe common factors associated with Roseomonas ocular infection and to point out some important considerations to be taken into account in its diagnosis and treatment.
Case Presentation
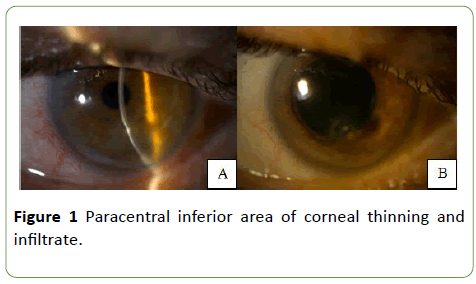
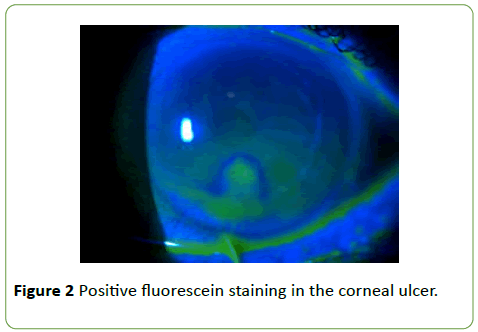
A 70-year-old diabetic man visited the ophthalmological emergency service of our center with complaints of photosensitivity, pain and blurred vision in the left eye for 4 weeks. By this time, the patient had already been consulted by an ophthalmologist and was under treatment with moxifloxacin 0.5%, clotrimazole 1%, prednisolone acetate 1% and oral valacyclovir hydrochloride 1g two times a day for 2 weeks. There was no history of trauma, previous ocular surgery or contact lens wearing and, furthermore, past ophthalmological history was unremarkable. On examination, best corrected visual acuity in the right eye was 20/20 and in the left eye 20/100. Examination of the right eye was unremarkable. The left eye presented with ciliary injection, mild flare and a paracentral inferior area of corneal thinning and infiltrate with 4 mm × 2.5 mm. No hypopyon was registered Figures 1 and 2 shows the bio-microscopy of the left eye.
Fundus details were unclear but B-scan echography revealed no vitreous echoes or retinal detachment. At this time, the patient stopped topical prednisolone and oral valacyclovir hydrochloride and continued the remaining medication previously ongoing. Corneal scrapings were sent for bacterial, fungal, viral and acanthamoeba culture.
Five days later, the cultures showed growth of a gramnegative bacillus, that could not be identified at that time, and were negative for fungal and acanthamoeba. Attending to these early results, the patient stopped clotrimazole 1% and was empirically treated with topical moxifloxacin 0.5% and tobramycin 0.3% every two hours. After three days, the culture was positive for a gram-negative bacillus, producing pink-pigmented raised colonies that were identified as Roseomonas gilardii .
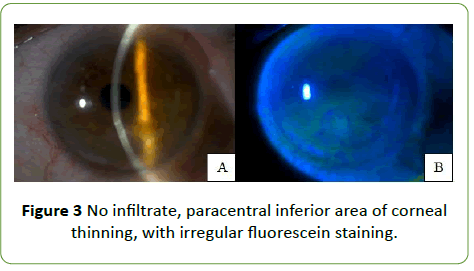
On day eleven, the patient reported subjectively better visual acuity in the left eye, less photosensitivity and no ocular pain. Slit lamp examination of the left eye Figure 3 revealed no flare, no corneal infiltrate and a decrease in the size of the corneal ulcer, however an important area of corneal thinning with peripheral corneal neovascularization. At this time, the patient remained under monitoring only with preservative-free, lubricant eye drops, 5 times per day.
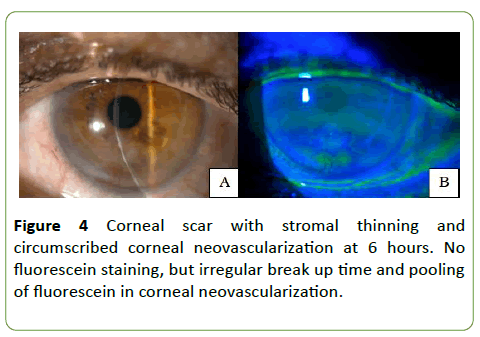
Four months later, visual acuity in the right eye was 20/20 with -0.50 diopters of astigmatism and of 20/25 in the left eye without correction. Biomicroscopy registered a corneal scar in the area of the previous ulcer with corneal stromal thinning and circumscribed corneal neovascularization in the left eye Figure 4. Intraocular pressure was 12 mmHg and fundoscopy was normal, bilaterally. The patient was asymptomatic and pleased with the recovery of the visual acuity in the left eye and was kept under treatment with lubricant eye drops.
Discussion
Roseomonas gilardii is a nonfermentive, pink-pigmented gram-negative coccobacillus belonging to the genus Roseomonas , first described by Rihs et al. [1]. Although Roseomonas species have been isolated from clinical samples, such as blood, and from environmental sources, such as water and soil, human infections caused by Roseomonas are particularly rare [2,3]. The species Roseomonas mucosa and Roseomonas gilardii have been the most reported as being associated with human infections including ocular infection, and a common finding in the literature is that human infection caused by this pathogen seems to be a feature of immunocompromised patients like those with malignancy, diabetes, on cancer chemotherapy, those with catheters, respiratory problems, wound infection, peritonitis or enteritis [3-7].
Bacteremia is the most common clinical presentation reported in the literature, however there are 4 previous reports of ocular infection due to the Roseomonas species: 2 infectious keratitis and 2 endophthalmitis. The first one was described by Tabin et al. presenting a corneal ulcer and infiltrate with hypopyon in an 82-year-old female patient who had been on daily topical steroid for 3 years [8]. The infection lead to corneal scarring after 7 weeks of treatment with target antibiotics, ending with a visual acuity of 20/400 in the involved eye. The second case of keratitis was reported by Goyal et al. in a corneal graft of an 83-year-old female, also in daily topical steroid for 8 years after a penetrating keratoplasty [9]. The infection leads to corneal perforation despite target therapy for 6 weeks, ending up in a new penetrating keratoplasty. There are also two cases of endophthalmitis with overall bad prognosis – one in an 83-year-old female patient with total retinal detachment, who ended up in phitisis bulbi, and other in a 74-year-old diabetic man with a subretinal abcess who reached a visual acuity of 20/400 [5,10].
Comparing to these previously reported findings, in this case the infection also involved an older age patient, with an underlying chronic illness – diabetes – without, however, any significant past ophthalmological history. Consistent with all reports, the pathogen revealed a slow-growth property on culture, taking 5 days to reveal the growth of a gram-negative bacillus and three more days to clearly be identified as Roseomonas gilardii .
However, in contrast with the previous reports of ocular infections, we presented a case where the patient achieved a good outcome after treatment with target topical antibiotics.
Besides all these reports, the clinical significance of Roseomonas ocular infection appears to remain uncertain as a result of its rarity. One important tool managing this infection seems to be the early identification of the pathogen to target therapy. In this patient, we did not test antibiotic susceptibility; however, antibiotic sensitivity pattern of Roseomonas has been largely studied [1-4].
Roseomonas have been reported to be susceptible to amikacin, gentamicin, tobramycin, tetracycline and ciprofloxacin, but rarely susceptible to penicillin and cephalosporins, including the extended-spectrum. There is no data on susceptibility to newer quinolones, but, in the literature, about 90% of the isolates were susceptible to ciprofloxacin and also to levofloxacin [4]. In this case, after culture results, and because the patient was already under treatment with topical moxifloxacin, we immediately targeted dual therapy by adding tobramycin. Six days later, there were no signs of an active infection. The patient achieved a visual acuity of 20/25 and revealed a small corneal scar in the area of the previously ulcer with corneal stromal thinning and circumscribed corneal neovascularization. Differently from the two previously reported cases of Roseomonas keratitis, the patient recovered well, with a very positive outcome. One of the possible explanations is that the isolated species was the Roseomonas gilardii instead of the Roseomonas mucosa, which had demonstrated a higher resistance to antimicrobial agents in the studies [3,4]. Besides that, the patient had been on topical moxifloxacin at least after two weeks from the beginning of the symptoms and we added tobramycin promptly after the culture results. We think that targeted dual therapy should be strongly considered after Roseomonas isolation due to the susceptibility pattern of this pathogen. Another possible reason is that our patient had an overall past ophthalmological history which was unremarkable, with no previous ocular surgeries and no evidence of topical steroids use. In the case of Goyal et al. the infection was in a corneal graft that, by itself, is a condition associated with increased inflammation, having a higher risk of progression to corneal perforation, graft dehiscence and subsequent failure [11]. Moreover, despite the fact that this infection seems to occur in debilitated patients, most of the literature reports on human infections, caused by Roseomonas , describe a complete recovery of patients with antibiotic treatment [3,4].
Conclusion
To summarize, Roseomonas infection induces an indolent infection which may result in misdiagnosis and delayed treatment. Corneal scrapers should be done promptly in corneal ulcers which are refractory to the treatment. It is important to pursue final identification of this pathogen because of its susceptibilities to antibiotics – therefore, we recommend considering gram-negative coverage with an aminoglycoside and quinolone. This organism usually causes infection in patients with any conditions which compromise the immune system of the eye, such as diabetic patients or patients on daily topical steroids. We think that reporting cases of rare pathogens is fundamental for ophthalmologists to improve their ability to recognize and effectively manage this type of infections.
Authors' Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All authors contributed to the draft of the manuscript, critically reviewed for intellectual content and approved the final version submitted for publication. LM and LO contributed to the acquisition of data and case report design. MN and MG contributed to critical interpretation of data.
References
- Rihs JD, Brenner DJ, Weaver RE, Steigerwalt AG, Hollis DG, et al. (1993) Roseomonas , a new genus associated with bacteremia and other human infections. J Clin Microbiol 31: 3275-3283.
- Han XY, Pham AS, Tarrand JJ, Rolston KV, Helsel LO, et al. (2003) Bacteriologic characterization of 36 strains of Roseomonas species and proposal of Roseomonas mucosa sp nov and Roseomonas gilardii subsp rosea subsp nov. Am J Clin Pathol 120: 256-264.
- Dé I, Rolston KV, Han XY (2004) Clinical significance of Roseomonas species isolated from catheter and blood samples: Analysis of 36 cases in patients with cancer. Clin Infect Dis 38: 1579-1584.
- Wang CM, Lai CC, Tan CK, Huang YC, Chung KP, et al. (2012) Clinical characteristics of infections caused by Roseomonas species and antimicrobial susceptibilities of the isolates. Diagn Microbiol Infect Dis 72: 199-203.
- Bhende M, Karpe A, Arunachalam A, Therese L, Biswas J (2017) Endogenous endophthalmitis due to Roseomonas mucosa presenting as a subretinal abscess. J Ophthalmic Inflamm Infect 7: 5.
- Shokar N, Shokar GS, Islam J, Cass AR (2002) Roseomonas gilardii infection: Case report and review. J Clin Microbiol 40: 4789-4791.
- Bello LJM, Trejo UI, Domínguez MCA, García CC, Medina JR (2015) Identification and molecular characterization of Roseomonas genomospecies 5 isolated from umbilical cord blood unit. Rev Med Hosp Gen Méx 80: 24-30.
- Tabin G, Danenhower C, Reardon D, Dimmig J, McCormick G (2001) Opportunistic Roseomonas keratitis. Cornea 20: 772-773.
- Goyal S, Warner D (2013) Roseomonas keratitis after remote penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol 251: 1025-1027.
- Chen KJ, Lai CC, Kuo YH, Wu WC, Chen TL (2008) Chronic postoperative Roseomonas endophthalmitis. J Clin Microbiol 47: 266-267.
- Vajpayee RB, Sharma N, Sinha R, Agarwal T, Singhvi A (2007) Infectious keratitis following keratoplasty. Surv Ophthalmol 52: 1-12.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences