Hemorrhage Due to Endotracheal Extubation in a Patient with Laryngeal Amyloidosis
Ceyhan H, Kesimci E, Erkilic E* and Aksoy SM
DOI10.21767/2471-8041.100090
Ceyhan H, Kesimci E, Erkilic E* and Aksoy SM
Faculty of Medicine, Department of Anesthesiology and Reanimation, Ankara Atatürk Training and Research Hospital, YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm BeyazÃÆââ¬Å¾Ãâñt University, Ankara, Turkey
- *Corresponding Author:
- Ezgi ErkÃÆââ¬Å¾ÃâñlÃÆââ¬Å¾Ãâñc
Faculty of Medicine, Department of Anesthesiology
and Reanimation, Ankara Atatürk Training
and Research Hospital, YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm BeyazÃÆââ¬Å¾Ãâñt University
Ankara, Park cd Rönesans evleri A-11
Çayyolu-Ankara, Turkey
Tel: 90 312 2912726
E-mail: eerkilic72@yahoo.com
Received Date: November 08, 2017 Accepted Date: November 22, 2017 Published Date: November 24, 2017
Citation: Ceyhan H, Kesimci E, Erkilic E, Aksoy SM (2017) Hemorrhage Due to Endotracheal Extubation In a Patient with Laryngeal Amyloidosis. Med Case Rep Vol.4 No.1:55. doi: 10.21767/2471-8041.100090
Abstract
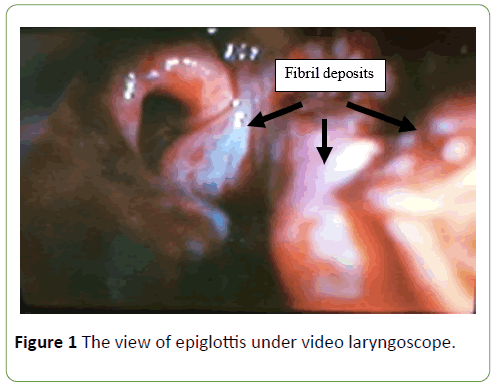
Amyloidosis is a disease characterized by deposition of proteins in tissues and organs. When these fibril deposits disrupting organ function confine to a single organ system, it is ''localized amyloidosis''. We herein; present a patient undergoing surgery for laryngeal amyloidosis located in neck region; to provide recommendations regarding the anesthetic management and follow-up of these patients. We wanted to call attention to the recurrent nature of this disease and the possibility of life threatening conditions that should be kept in mind in order to take precautions on time.
Keywords
Amyloidosis; Laryngeal; Airway; Hemorrhage
Introduction
Amyloidosis is a disease characterized by deposition of proteins in tissues and organs, affecting mostly respiratory, urogenital, and gastrointestinal tract as well as the skin [1,2]. Clinically, amyloidosis is divided into two main types, namely systemic and localized [3]. In ''systemic amyloidosis'', prognosis is poor due to systemic involvement with clinical symptoms such as proteinuria with nephrotic syndrome, peripheral neuropathies, dementia and cognitive dysfunction and enlargement of the liver, kidney, spleen and heart [4].
When fibril deposits disrupting organ function confine to a single organ system, it is called ''localized amyloidosis''. Localized amyloidosis in the neck and head is a benign disease but tends to recur. If localized amyloidosis of neck is symptomatic; causing dyspnea, obstruction, hemorrhage or dysfunction, conservative surgery is essential. Follow up of these patients are recommended yearly. Laryngeal amyloidosis affecting mostly vocal cords and ventricles is relatively rare [2].
We herein; aimed to call attention to anesthetic management and follow-up of patients undergoing recurrent surgery for unexpected complications in laryngeal amyloidosis.
Case Report
A 60-year-old male patient with complaints of respiratory distress was hospitalized for excision of mass in the neck. He had laryngeal amyloidosis diagnosed seven years ago. His rectal and upper gastrointestinal biopsies were negative for amyloidosis. He had uneventful general anesthesia experience for tonsillectomy last year.
At the preoperative evaluation, there was nothing remarkable, except for mild dyspnea and dysphagia due to mass on the neck and heavy smoking given up recently. Routine laboratory tests and echocardiogram were normal. On direct laryngoscopy; vocal cord movements were normal and there were inter-arytenoepiglottic amyloid deposits (Figure 1). He came to the operating room with preoperative corticosteroid prophylaxis. General anesthesia was induced with propofol (2 mg.kg-1) and rocuronium bromide (0.6 mg.kg-1) after standard monitorization and maintained with desflurane (6 vol%), with a fresh gas flow rate of 3 L/min and 50% oxygen in air and intravenous remifentanil infusion. The patient was intubated with 8 mm cuffed endotracheal tube via laryngoscopy using a Macintosh blade (No. 3) without inducing any trauma and then mechanically ventilated. Bilateral neck dissection was performed.
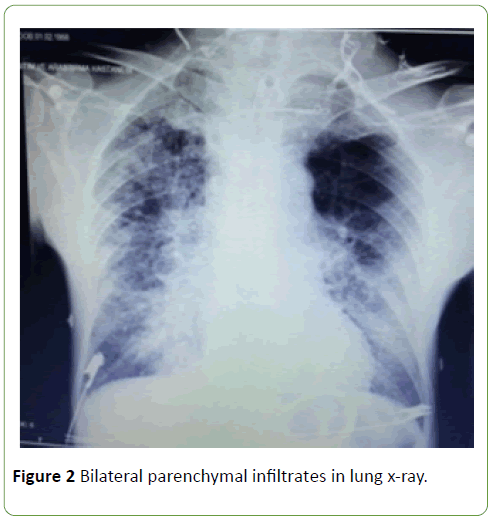
The operation lasted 1 hour and 30 minutes in total. After the reversal of muscle relaxation, fresh blood was noted refluxing from the endotracheal tube and tracheobronchial suction was gently performed with 14 Fr. catheter. No intraoral bleeding was observed. Once his ventilation and conscious state were satisfactory, he was extubated. However, he immediately developed airway obstruction with inspiratory stridor. Anticipating a difficult intubation, a smaller diameter endotracheal tube (6.5 mm) via videolaryngoscope was inserted. Subsequently, the presence of airway injury due to endotracheal intubation was searched and hemostasis was achieved using gauze around the larynx moistened with 1:1000 epinephrine solution under direct laryngoscopy. As the amount of bleeding decreased gradually he was extubated safely. His oxygen saturation remained around 94-96% by nasal O2 and cold steam during his one-hour follow-up in the Post Anesthesia Care Unit. He was then transferred to surgical ward without any respiratory abnormality being noticed by the anesthesiologist. However, he had respiratory failure after 8 hours, thus this time emergent tracheotomy was performed. Then he was followed by supplemental O2 with bed rest. On 4th post-operative day; he was transferred to intensive care unit where he was placed on mechanical ventilation and treated with positive end-expiratory pressure (PEEP) due to respiratory failure developing as a result of bilateral parenchymal infiltrations (Figure 2). By appropriate antibiotherapy and proper ventilatory adjustments, he had an uneventful recovery and was discharged to the surgical ward on day 24th post-operative day. For this presentation, we received consent from the patient.
Discussion
Laryngeal amyloidosis, classically caused by either systemic or localized amyloidosis, is slowly progressive [5]. Its management requires close follow-up to exclude recurrence and not to miss surgical excision of the amyloid deposits if they recur. In this case, we tried to call attention to potentially fatal complication of localized amyloidosis of the larynx due to an intractable upper airway hemorrhage that an anesthesiologist might face during endotracheal intubation and extubation.
Amyloidosis is a heterogeneous group of disorders characterized by abnormal protein formation and deposition showing apple-green birefringence under polarized light on Congo red staining [5,6]. Clinically it is divided into two main categories as systemic and localized. In systemic amyloidosis, amyloid is accumulated mainly in kidney, liver, spleen and heart leading to dysfunction of these organs. Life expectancy is shortened with systemic involvement [3]. On the other hand, localized amyloidosis is usually benign and appears during the fifth and/or sixth decade of life. The larynx is the most common site of localized amyloidosis. In clinical presentation, hoarseness of the voice is the most common symptom [7]. Due to enlargement of the organs or tissues in the neck, patients also suffer from dysphonia, dysphagia and dyspnea [8]. As laryngeal amyloidosis is fragile and hemorrhagic, massive bleeding may occur during intubation. Chow et al. documented cases of fatal upper airway hemorrhage and obstruction due to the laryngeal lesion [9]. A proper preoperative evaluation of the airway of these patients as well as formulating the anesthetic plan for management of airway difficulties for anesthesiologists is important [8]. The aim of therapeutic options for localized laryngeal amyloidosis is to obtain a long disease-free interval without symptoms with various modalities of surgery [10]. Complete excision is usually preferred. However; if radical excision would increase the risk of scarring, dysphonia, or dysphagia; debulking of the amyloid deposits is performed. The surgical modalities are adapted according to the localization. Also, CO2 laser and micro debrider are used in other parts of the larynx or in bulky amyloid [11-14].
Another challenging issue is requirement of repeated resections after initial surgery, because recurrence occurs almost in all patients [15]. Our patient had two previous operations as a result of mass in the neck in one of which he had tracheotomy for airway security. Hazenberg et al. reported that two-thirds of their patients needed revision surgery, such that half of them had been within 1 year after initial surgery. They recommended a follow-up of 7 years since last surgery because progression of the disease was determined to come to a stop after 7 years [16]. The patient in our case, also gave the same history with regard to duration of his disease. However, on 7th year, he needed a revision surgery.
Anesthesiologists should have a high degree of suspicion about the possibility of difficult intubation and complications related to the airway, in these patients. Urgent airway management may be required often within a multidisciplinary team including anesthesiologist and otolaryngologists. During induction maintaining spontaneous ventilation without muscle relaxant may be considered as appropriate technique. It is recommended that fiberoptic bronchoscopy and tracheostomy be prepared in case of difficult airway. Also, various sizes of tracheal tubes should be prepared. The patient should be monitored in the intensive care unit postoperatively because obstruction can occur at emergence and extubation [8].
Conclusion
Though laryngeal amyloidosis is a benign disorder, up to date, there has been no exact curable treatment. If complete excision is proved to be with high morbidity, patients should be followed on a yearly basis. On the other hand, the patients sometime may be fatal as a result of upper airway obstruction and respiratory failure [17]. In the clinical approach of these patients, it must be proven that it is not systemic amyloidosis [10]. Anesthesiologists should take care in intubating and extubating the tracheas of these patients and be aware of other systemic involvements.
In conclusion, this case demonstrated the fate of a patient due to development of hemorrhage and respiratory failure following recurrent surgeries for amyloidosis. Thus, the possibility of life threatening conditions should be kept in mind and precautions should be taken.
References
- Stevenson R, Witteles R, Damrose E, Arai S, Lafayette RA, et al. (2012) Arch Otolaryngol Head Neck Surg 138: 509-511.
- Tulunay O, Dursun G, Beton S, Erinç H, Batikhan H (2007) Amyloidosis of the larynx: A case report. Kulak Burun Bogaz Ihtis Derg 17: 40-43.
- Bozkus F, Ulas T, Lynen I, Ozardali I, Sans I (2013) Primary localised laryngeal amyloidosis. J Pak Med Assoc 63: 385-386.
- Park JH, Cheng HM (2013) Isolated laryngeal amyloidosis in a patient with a hoarse voice. BMJ Case Rep 5.
- Wierzbicka M, BudzyÃÆââ¬Â¦Ãâââ¬Å¾ski D, Piwowarczyk K, Bartochowska A, MarszaÃÆââ¬Â¦Ãâââ¬Å¡ek A, et al. (2012) How to deal with laryngeal amyloidosis? Experience based on 16 cases. Amyloid 19: 177-181.
- Rudy SF, Jeffery CC, Damrose EJ (2017) Clinical characteristics of laryngeal versus nonlaryngeal amyloidosis. Laryngoscope.
- Biewend ML, Menke DM, Calamia KT (2006) The spectrum of localized amyloidosis: A case series of 20 patients and review of the literature. Amyloid 13: 135-142.
- Noguchi T, Minami K, Iwagaki T, Takara H, Sata T, et al. (1999) Anesthetic management of a patient with laryngeal amyloidosis. J Clin Anesth 11: 339-341.
- Chow LT, Chow WH, Shum BS (1993) Fatal massive upper respiratory tract haemorrhage: an unusual complication of localized amyloidosis of the larynx. J Laryngol Otol 107: 51-53.
- Bartels H, Dikkers FG, Van der Wal JE, Lokhorst HM, Hazenberg BP (2004) Laryngeal amyloidosis: localized versus systemic disease and update on diagnosis and therapy. Ann Otol Rhinol Laryngol 113: 741-748.
- Motta G, Salzano FA, Motta S, Staibano S (2003) CO2-laser treatment of laryngeal amyloidosis. J Laryngol Otol 117: 647-650.
- Paccalin M, Hachulla E, Cazalet C, Tricot L, Carreiro M, et al. (2005)Localized amyloidosis: A survey of 35 French cases. Amyloid 12: 239-245.
- Dedo HH, Izdebski K (2004) Laryngeal amyloidosis in 10 patients. Laryngoscope 114: 1742-1746.
- Piazza C, Cavaliere S, Foccoli P, Toninelli C, Bolzoni A, et al. (2003) Endoscopic management of laryngo-tracheobronchial amyloidosis: A series of 32 patients. Eur Arch Otorhinolaryngol 260: 349-354.
- Gean-Marton AD, Kirsch CF, Vezina LG, Weber AL (1991) Focal amyloidosis of the head and neck: evaluation with CT and MR imaging. Radiology 181: 521-525.
- Hazenberg AJ, Hazenberg BP, Dikkers FG (2016) Long-term follow-up after surgery in localized laryngeal amyloidosis. Eur Arch Otorhinolaryngol 273: 2613-2620.
- Wang Q, Chen H, Wang S (2014) Laryngo-tracheobronchial amyloidosis: A case report and review of literature. Int J Clin Exp Pathol 7: 7088-7093.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences