Embolization of a giant splenic artery aneurysm
André Lollert,
André Lollert1*, Roman Kloeckner1, Friedrich Dünschede2, Christoph Düber1 and Michae1 Bernhard Pitton1
1Department of Diagnostic and Interventional Radiology, Medical Centre of the Johannes Gutenberg University, Mainz, Germany.
2Department of Cardiothoracic and Vascular Surgery, Medical centre of the Johannes Gutenberg University, Germany
- *Corresponding Author:
- André Lollert
Department of Diagnostic and Interventional Radiology
Medical Center of the Johannes Gutenberg University Langenbeckstr, Germany
Tel: +49-6131-172019
E-mail: andre.lollert@unimedizin-mainz.de
Received date: February 08, 2016; Accepted date: April 15, 2016; Published date: April 24, 2016
Citation: Lollert A, Kloeckner R, Dünschede F. Embolization of a Giant Splenic Artery Aneurysm. Med Case Rep. 2016, 2:2.
Abstract
Background Splenic artery aneurysms (SAA) are the most frequent visceral artery aneurysms. Large and symptomatic aneurysms have an increased risk for rupture and should be treated interventionally or surgically. Methods We describe the case of a 44-year-old male patient with a possibly mycotic splenic artery aneurysm of approximately 12 cm in diameter. Results As a result of a consensus in an interdisciplinary case discussion, endovascular embolization was successfully performed. No late complications occurred during a 3- year follow-up. Conclusion Minimal-invasive percutaneous transcatheter embolization was an effective and safe treatment for a large SAA. As there are no evidence-based guidelines, the decision whether to treat interventionally or surgically must be made individually.
Keywords
Aneurysms; Splenic artery; Amplatzer; Fibre; Microcatheter
Introduction
As the use of computed tomography and magnetic resonance imaging of the abdomen is increasing, the detection rate of clinically silent splenic artery aneurysms (SAA) has become higher than in the past. The exact etiology of SAAs is unknown. They may be associated with other medical conditions such as hypertension, obesity, atherosclerosis or liver cirrhosis [1]. There seems to be an increased risk in patients with portal hypertension [2]. It is generally recommended that SAAs larger than 2 cm in diameter should be treated to avoid rupture, although there are no randomized studies, which confirm this cut-off. There is a strong recommendation to treat symptomatic aneurysms. Other factors such as liver cirrhosis or planned liver transplant and alpha-1-antitrypsin deficiency are also considered important, but with less evidence [1]. Mycotic aneurysms have an increased rupture risk and should therefore be treated as well [3]. The purpose of this case report is to show that minimal-invasive percutaneous transcatheter embolization is an effective and safe treatment option even for large and possibly mycotic SAAs.
Case Presentation
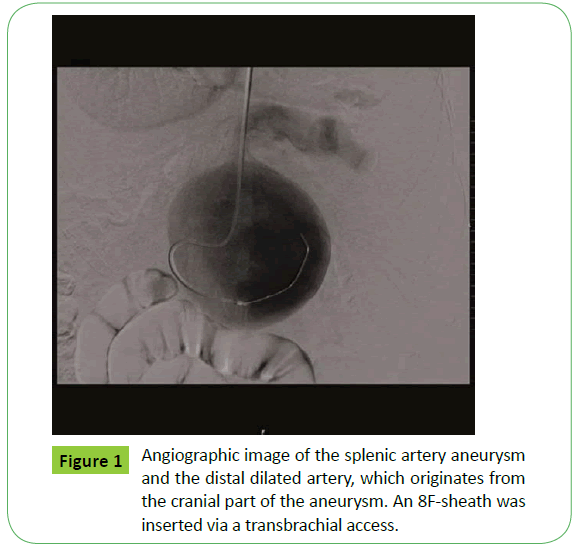
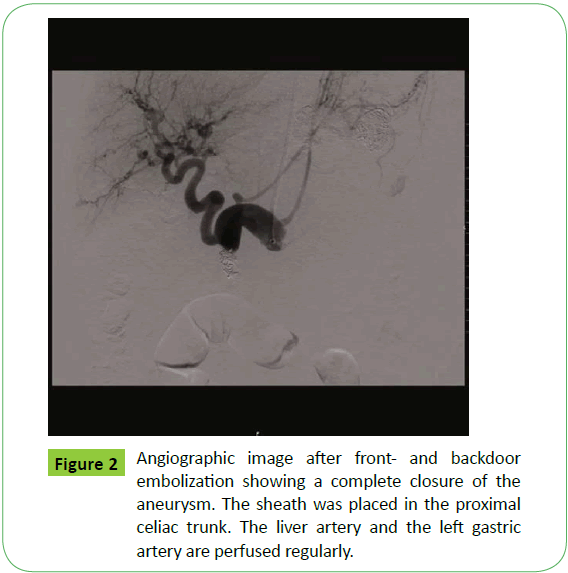
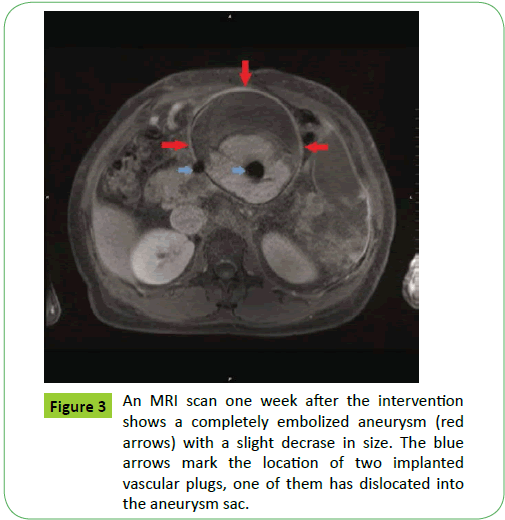
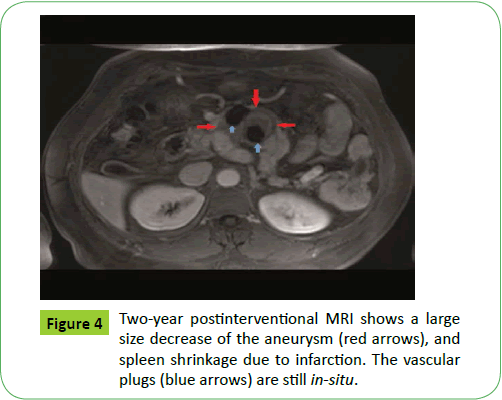
A 44-year-old male patient was referred to our University Medical Center in January 2013 presenting with a giant splenic artery aneurysm. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. Considerable pulsation could be palpated in the upper middle abdomen. The patient described slight abdominal pain and presented with an icterus (bilirubin serum level was 16 mg/dl) and infect constellation (c-reactive protein [CRP] was elevated up to 129 mg/l, white blood cells [WBC] ranged from 8.87 to 11.2/nl). Multiple bleedings from gastro esophageal varices due to portal vein thrombosis had occurred during childhood. At the age of 17 years, a surgical mesenterico-caval H-shunt was applied due to persisting portal hypertension. A hepatitis B infection occurred as a transfusion complication. Computed tomography and magnetic resonance imaging showed a SAA measuring approximately 12.5 x 11.5 x 12.5 cm. The distal part of the artery was dilated with a diameter of about 4 cm. The spleen was enlarged to 19.1 x 6.2 x 18 cm and showed several areas with minor perfusion, most probably as a result of splenic infarcts. No other infect focuses than the aneurysm itself (possibly mycotic) or an improbable superinfection of the infarcted splenic areas could be found. Surgical treatment was not performed due to the risk of intraoperative aneurysm rupture and injuries of the massive portocaval collaterals which resulted from long-time portal hypertension. A transcatheter approach was indicated, even though a mycotic aneurysm was possible. Because of the vascular anatomy (steep celiac trunk), a transbrachial access via the left cubital artery was chosen. An 8F-sheath was introduced to the SAA. Angiography confirmed the giant aneurysm, the distal splenic artery was also considerably dilated (Figure 1). A 5F-catheter and coaxial microcatheter were placed into the middle third of the distal splenic artery. Embolization was performed using 25 micro-coils with diameters between 10 and 17 mm (Platinum Coil, Boston Scientific GmbH, Ratingen, Germany). In addition, nine interlock coils (Boston Scientific GmbH) were introduced in order to create a stable and tight cluster of coils. As the subsequent angiography still showed a relevant blood flow, additional embolization with an emulsion of n-butyl-2-cyanoacrylate (Histoacryl®, B. Braun AG, Melsungen, Germany) and ethiodol (Lipiodol® Ultra-Fluid, Guerbet GmbH, Sulzbach, Germany) in a proportion of 1:2 was performed to entangle in the coils for a complete occlusion of the artery for backdoor closure. The aneurysm sac itself remained untouched since no arteries for potential backflow could be detected during selective contrast bolus injection and because of its grand volume. The aneurysm neck was occluded using a 16 mm Amplatzer™ Vascular Plug II (St. Jude Medical GmbH, Eschborn, Germany), after a 14 mm plug had dislocated into the aneurysm sac. Two 10 mm interlock coils were placed next to the plug, which led to complete closure of the splenic artery, while the celiac trunk, the liver artery, and the left gastric artery were still perfused regularly (Figure 2). After manual compression of the cubital artery, a regular blood flow in the brachial artery was demonstrated by ultrasound, whereas the radial and ulnar artery showed a weak blood flow. A vascular surgical exploration of the brachial artery was performed for thrombectomy; the artery was closed with a venous patch after the procedure. There were no clinical signs of a hand ischemia after the operation. The patient could be discharged home on the 10th postinterventional day. CRP and WBC dropped to normal levels under antibiotic therapy after the intervention and stayed low during follow-up. MRI scans one week (Figure 3), two months, and five months after the intervention showed a completely thrombosed aneurysm with a slight decrease in size and splenic infarction. Nine months postinterventional MRI showed a large size decrease of the aneurysm to approximately 4.1 x 4.6 x 4.4 cm, as well as spleen shrinkage due to infarction. A two-year follow-up MRI scan documented a further shrinkage of the still completely thrombosed aneurysm to approximately 3.9 x 3.4 x 3.4 cm (Figure 4). A further regression to approximately 3.8 x 3.0 x 3.0 cm was demonstrated in an MRI examination three years after the intervention.
Discussion
Splenic artery aneurysms are the most common visceral artery aneurysms and account for up to 60% of all visceral artery aneurysms. These aneurysms sometimes present as emergencies with life threatening rupture, however most aneurysms are incidental findings. They are asymptomatic in about 75% of cases and frequently detected by CT and MRI performed due to other reasons. SAAs are associated with general and portal hypertension, obesity, atherosclerosis or liver cirrhosis. Most aneurysms are smaller than 2 cm, and they are multiple in 20% of cases. The risk for rupture ranges from 3 to 10% [1]; mycotic aneurysms have an even higher risk [3]. Ruptured SAAs have a high mortality, so at the moment there are several recommendations for treatment: Size larger than 2 cm, aneurysms in patients with liver cirrhosis or undergoing liver transplant, aneurysms in patients with alpha-1- antitrypsin deficiency, and aneurysms in pregnant women or in women of childbearing age [1]. Despite these recommendations, there are no randomized studies to confirm these indications. Clinical experience at our institution shows that the risk of rupture is not solely correlated with the aneurysm size, which was also confirmed by others [4]. The only clear consensus is that symptomatic SAAs should be treated immediately [5], since rupture can result or has already occurred, leading to a high mortality. SAAs can be treated surgically with a ligation of the splenic artery, ligation of the aneurysm or aneurysmectomy (sometimes including splenectomy) and with an open or laparoscopic operation [6]. Interventional treatment has emerged as a treatment of choice and the efficacy and safety of this method has been demonstrated [7-9]. However, due to a low overall incidence, evidence-based data is lacking. Treatment decisions are therefore commonly based on clinical experience of the interventional radiologist or vascular surgeon. As presented in our case, even large and possibly mycotic SAAs can be treated safely with a catheter-based intervention. Compared to surgery, the main advantage is that most interventions can be performed in local anesthesia with a high technical success rate and a fast recovery after a short length of stay in the hospital [9].The technique for embolization varies in literature, most institutions use coils as embolization material, sometimes, as presented in our case, in combination with glue. Techniques also vary between embolization of the aneurysm sac itself [10], which is only possible in small or medium sized SAAs, and, as presented here, embolization of the in- and outflow vessels [11]. It has been shown that if the aneurysm sac cannot completely be filled with coils, there is an increased risk for a continued aneurysm flow [10]. We could show that embolization of the in- and outflow vessels was an effective technique and should therefore be taken into consideration especially in cases with very large aneurysms. In our case, aneurysm expansion and rupture was successfully avoided during three years of follow-up. Adverse events can be either procedure-related (e. g. splenic infarct, non-target embolization, splenic artery dissection) or access-site related, most probably due to a large sheath size, which was necessary in our case due to a very steep celiac trunk. This complication could be resolved with minor surgery in our case. In conclusion, each case of SAA should be discussed individually and treatment decisions should be based on patient anatomy, size of the aneurysm and general patient condition. At the moment there are no controlled randomized trials comparing the surgical and the interventional approach. However, the minimalinvasive approach of catheter-based treatment has demonstrated technical success and safety, even in this giant splenic artery aneurysm.
References
- Abbas A, Stone M, Fowl R, Gloviczki P, Oldenburg A, et al. (2002) Splenic artery aneurysms: two decades experience at Mayo clinic. Ann Vasc Surg 16: 442-449.
- Carroccio A, Jacobs S, Faries P, Ellozy H, Teodorescu J et al. (2007) Endovascular treatment of visceral artery aneurysms. Vasc Endovascular Surg 41: 373-382.
- Eng W, Venkatesh K (2010) Clinics in diagnostic imaging (131). Multiple visceral mycotic aneurysms. Singapore Med J 51: 824-829.
- Sessa C, Tinelli G, Porcu P, Aubert A, Thony F et al. (2004) Treatment of visceral artery aneurysms: Description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg 18: 695-703.
- Carr SC, Pearce WH, Vogelzang RL, McCarthy WJ, Nemcek AA Jr et al. (2001) Visceral artery aneurysm rupture. J Vasc Surg 33: 806-811.
- Kim Y, Johna S (2013) Laparoscopic excision of splenic artery aneurysm. JSLS 17: 132-134.
- Fankhauser T, Stone M, Naidu G, Oderich S, Ricotta J et al. (2011) The minimally invasive management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg 53: 966-970.
- Pitton B, Dappa E, Jungmann F, Kloeckner R, Schotten S et al. (2015) Visceral artery aneurysms: Incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol 25: 2004-2014.
- Lakin O, Bena F, Sarac P, Shah S, Krajewski P et al. (2011) The contemporary management of splenic artery aneurysms. J Vasc Surg 53: 958-964.
- Patel A, Weintraub J, Nowakowski F, Kim E, Fischman M et al. (2012) Single-center experience with elective transcatheter coil embolization of splenic artery aneurysms: technique and midterm follow-up. J Vasc Interv Radiol 23: 893-899.
- Widlus M, Moeslein M, Richard M (2008) Evaluation of the Amplatzer vascular plug for proximal splenic artery embolization. J Vasc Interv Radiol 19: 652-656.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences