Clinical and Dermoscopic Features of Nevi in Patients with Vitiligo
Deeva N, Ilina N, Krinitsyna M, Taganov A, Kolesnikova S, Yudkin D and Sergeeva G.
Deeva N1*, Ilina N1, Krinitsyna M1,2, Taganov A1, Kolesnikova S3,Yudkin D3 and Sergeeva G1,4
1Medical Department, Novosibirsk State University, Novosibirsk, Russia
2Novosibirsk Research Institute of Regional Pathology and Path Morphology, Novosibirsk, Russia
3Chromosome Pathology Group, Institute of Molecular and Cellular Biology, SB Russian Academy of Science,Novosibirsk, Russia
4Laboratory of Translational Brain Research, Institute of International Tomography, Center of the Russian Academy of Sciences, Novosibirsk,Russia
- *Corresponding Author:
- Natalia Deeva
Medical Department, Novosibirsk State University, Novosibirsk, Russia
Tel: +79134790601
E-mail: pikelgaupt1991@gmail.com
Received date: January 27, 2016; Accepted date: June 23, 2016; Published date: June 27, 2016
Citation: Deeva N, Ilina N, Krinitsyna M, et al. Clinical and Dermoscopic Features of Nevi in Patients with Vitiligo. Med Case Rep. 2016, 2:2.
Abstract
The aim of the study was to display clinical and dermatoscopic features of melanocytic nevi among patients with Vitiligo.
Materials and methods: This study was conducted in 37 patients with Vitiligo (8 male and 29 female patients from 12 to 77 years of age). Clinical histories of all patients were reviewed in detail: age, sex, duration of disease, anatomic site affected, full body photometric skin examination, dermoscopy examination on the dermatoscope HEINE MINI 10X with 70% ethyl alcohol immersion and nevi assessment according to Pehamberger pattern analysis were obtained for all recruited patients.
Results: Following dermoscopic features of melanocytic nevi in Vitiligo patients were noted: hypopigmentation, depigmented globules, fragmented pigment network and vascular pattern. The most frequent dermoscopy pattern was structure less areas (74%). In a half of all nevi globules (51%) and hypo pigmented areas (47%) were seen. In 12.5% of globular nevi globules with central hypopigmentation were observed that looked like pigment circles.
Conclusion: It is important to notice that depigmentation in patients with Vitiligo can be observed not only as skin patches, but also as a dermoscopy feature in melanocytic nevi, that is not any pathology nor any sign of dysplasia but only the sign of the autoimmune reaction against the pigment.
Keywords
Melanocytic nevi; Vitiligo; Dermoscopy
Background
Vitiligo is a common skin disease characterized by autoimmune melanocyte destruction. However, the interaction of autoantibodies and pigment-containing cells is not well understood. Certain cases of recourse pigmentation in congenital nevi prior to the beginning of the disease, emergence of the halo area around the postoperative scar after the removal of a congenital nevus and a case of simultaneous repigimentation of a halo nevus and areas of Vitiligo were described [1-4].
About 20% of patients with Vitiligo have halo nevi. The presence of halo nevi is one of the risk factors of disease progression [5]. Halo nevi have a strict association with Vitiligo and may be precursors or markers of the disease. According to data of European researchers [6], patients with multiple halo nevi have higher risk of developing of Vitiligo and other autoimmune diseases compared with patients with a single halo nevus. Among other types of melanocytic nevi few cases of Vitiligo and a blue nevus, Vitiligo and Ota’s nevus were described [7,8].
Melanocytic nevi are benign tumors of melanogenic system, where melanocytes tend to melanoma development. Melanoma can arise from melanocytic nevi or on intact skin. Dysplastic or atypical melanocytic nevi are considered to be an important factor associated with increased risk of cutaneous melanoma development [9,10]. Ultraviolet (UV) radiation (both natural and artificial) produces the highest risk of dysplasia appearance and further melanoma development [11].
Patients with Vitiligo are of greatest interest because they receive UV therapy, such as narrowband phototherapy 311 nm, PUVA (Psoralen plus UVA) and excimer laser therapy [12]. Nowadays dermoscopy is considered to be the most efficient tool for early melanoma diagnostics. It reduces the frequency of unreasonable biopsy and is efficient for nevi monitoring within the group of patients with Vitiligo as the frequency and precise dermatoscopic markers of nevi have not been yet thoroughly studied [13]. At the same time, the structure and dermatoscopic features of melanocytic nevi in Vitiligo patients are currently not well understood. The purpose of the study was to display clinical and dermatoscopic features of melanocytic nevi in patients with Vitiligo.
Materials and Methods
The first step of the study was to recruit 40 patients with Vitiligo. All patients had implications corresponding to criteria of the disease at the time of survey. Clinical histories of all patients were reviewed in detail: age, sex, duration of disease, anatomic site affected.
The second step of the study was to recruit 37 patients with Vitiligo (8 male and 29 female patients with the average age of 37.9 yrs). Three patients from the observed group were excluded from the further study on personal grounds. Clinical and dermatoscopic features of the nevi were reviewed: their localization, size and quantity. Complete questionnaire and full body photometric skin analysis, dermoscopy examination on the dermatoscope HEINE MINI 10X with 70% ethyl alcohol immersion and nevi assessment according to Pehamberger pattern analysis were obtained for recruited patients.
Results
Clinical characteristics
12 male and 28 female patients with Vitiligo ranging in from 8 to 77 years participated in the study. The mean duration of disease was 16.5 ± 2.3 years. At the first phase of the study, clinical features of Vitiligo in 40 patients were defined. The generalized Vitiligo form was observed in 21 patients (52.5%), mixed form – in 9 patients (22.5%), acrofacial and universal forms – in 3 patients (7.5%), focal and segmental forms – in 2 patients (5.0%). The progressing type of Vitiligo was revealed in 34 patients (85.0%), stable and unstable – in 3 patients (7.5%).
Vitiligo patches were most often located: on the back of brushes in 28 of the 40 cases (70.0%), on eyelids and axillary areas – in 24 (60.0%), on the breast, forearms and the back of feet – in 21 (52.5%), on the crus – in 20 (50.0%). Depigmented patches were less often found on chins, lips, buttocks, shoulders - in 8 (20.0%) patients, on cheeks - in 6 (15.0%). On the back and laps patches were found in 18 (45.0%) cases, on elbows - in 17 (42.5%), on inguinal folds - in 15 (37.5%), on huckles – 14 (35.0%), on the neck - in 11 (27.5%) cases.
Leucotrichia was found in 8 patients (20.0%). 4 from 40 patients with Vitiligo (10.0%) had a leucotrichia on pilar parts of the head, on the chin and eyelashes decoloured hair were found in 2 cases (5.0%), in axillary area, area pubis and on brows – on one patient (2.5%). On three patients leucotrichia combination was identified on the shin, in armpits and in pubic area, on the scalp, eyelashes and chin. All patients with leucotrichia had a nonsegmental form of Vitiligo (the mixed form – 5 patients, generalized – 2 and universal – 1), the progressing type was revealed in 6 patients and unstable – in 2.
Clinical characteristics of melanocytic nevi
Clinical and dermatoscopic features of nevi were reviewed: their localization, size and quantity. 83.8% of patients with Vitiligo had melanocytic nevi more than 4 mm in diameter (95 nevi totally). 30 nevi (31.6%) were localized on the back, 16 nevi (16.8%) – on top extremities, 15 nevi (15.8%) – on the breast and the stomach, 11 nevi (11.6%) – on the face, 9 nevi (9.5%) – on lower extremities. The majority of nevi had a diameter of 4 – 5 mm, in two patients (5.4%) two medium congenital nevi were found, 6 and 15 cm in diameter, of brown color, with a warty surface and hypertrichosis (Figure 1).
Among the main types of clinical nevi dermal acquired and mixed nevi were most commonly observed, which were presented as hemispherical or spherical papules, flesh-, light- and darkbrown colored, of soft-elastic consistency. In 7 patients (18.9%) 11 halo nevi were found, which were presented as papules of hemispherical shape, light-brown or flesh-colored, surrounded by erythematous depigmented halo. In most cases halo nevi were located on the back (64.0% of cases), in other cases – on the breast. In 3 patients (8.1%) observed a melanocytic nevus was revealed in the patches of Vitiligo. Multiple melanocytic nevi were observed in two male patients (Figure 2).
Dermatoscopic characteristics
Typical pigment network, which was characterized by a light to dark brown pigmented, regularly meshed and narrowly spaced network distributed more or less regularly throughout the lesion and usually thinning out at the periphery, was found in 30 cases (31.6%). Pseudo-network pigment, which was an option of a typical pigment network with localization on the face where cells of the network were follicles, was found in 4 cases (4.2%).
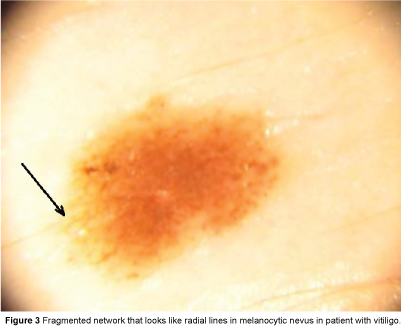
Structureless areas of light-brown or pink pigmentation, that precludes recognition of more subtle dermoscopy features, were found in 70 cases (73.7%). Structureless areas had a lower degree of pigmentation intensity compared with others and alternated or combined with hypopigmented areas in 45 cases (47.4%). It was also noticed in these combined nevi, that the pigment network was fragmented and was seen like radial lines or pseudopods at the periphery (Figure 3).
Another frequent dermatoscopic pattern was presented as globules of dark-brown or light-brown color, sharply circumscribed structures of a round or an oval shape, equal in size and distribution in the skin lesion. Globules were found in 48 nevi (50.5%) in Vitiligo patients.
While assessing the dermatoscopic features among Vitiligo patients, new dermatoscopic structure was found, which dermoscopic characteristics were: structureless hypopigmented areas, globules and circles. It is of interest that the “circles” were originally the globules, which central part was depigmented with time (“post-globule circles”). These structures were found in acquired dermal and combined (Figure 4) as well as in congenital nevi in 6 cases (12.5%). Vascular pattern, which was characterized by dermal vessels and erythema, was found in 29 cases (31%).
Summary and Discussion
The result of our study showed that 83.8% of patients with Vitiligo had melanocytic nevi more than 4 mm in diameter. 31.6% of nevi were located on the back. As for the Pehamberger analysis, melanocytic nevi corresponded to the following criteria: dermal nevus with a central hypopigmentation, ÃÆââ¬ËÃâÃÂompound melanocytic nevus, which appears as reticular/ granular model with the typical pigment network and hypopigmentation.
In this study, patients with Vitiligo most commonly had acquired dermal and combined nevi. Additionally, there were 18.9% cases of halo nevi, 5.4% cases of middle-sized congenital nevi. Dysplastic nevi, which appear as reticular/ granular model with the typical or atypical pigment network, regular or irregular dots/ granules, regular streaks, blots and diffuse hypopigmentation, were not found. There were no cases of dysplastic nevi among our Vitiligo patients. One patient with multiple melanocytic nevi had hypopigmentation, which was observed in all formations, indicating the uniformity of structure dermatoscopic nevi.
The question of the risk of dysplasia and melanocytic cancer development among Vitiligo patients was discussed in the literature for a long time. Thus, according to results of population studies among more than 10 thousand patients with Vitiligo, phototherapy treated patients had significantly increased risk of both types of skin cancer. However, according to the results of other authors, Vitiligo patients had a three times lower risk of melanoma and non-melanoma skin cancer (NMSC) despite receiving high doses of ultraviolet radiation previously [14,15]. Some results show that patients with Vitiligo have a decreased risk of melanoma and NMSC development during their lifetimes and suggest that phototherapy does not increase that risk [16].
While autoimmunity seen in Vitiligo patients may protect against melanoma development, the lack of protective melanin in these patients can lead to greater photodamage and an increased risk of melanoma and NMSC [17]. In our study 85% of patients with Vitiligo had progressive form of the disease which points to an active autoimmune process. Since the malignant potential of melanocytes from Vitiligo patients has not been studied, the question remains about the possible increase in the risk of dysplasia and melanoma development affected by UV therapy.
There are probably several mechanisms to explain the negative association between Vitiligo and skin cancer. First of all, this is the role of an anti-melanocytic immune response in Vitiligo patients; it is theoretically unlikely that melanoma would form in Vitiligo lesions because melanocytes are absent in these lesions; in Vitiligo patients overproduction of proinflammatory cytokines, such as interleukin-1 and tumour necrosis factor alpha (TNF-α), takes place, which stimulate the production of superoxide dismutase and glutathione peroxidase thus reducing the risk of skin cancer [18]. An isolated case of melanoma regression in 53-year-old patient with Vitiligo was described, in which the primary focus was not detected, and the diagnosis of melanoma was set for the detection of metastases in the lymph nodes [19].
In our study the most typical dermatoscopic picture of nevi in patients with Vitiligo was structure less areas (73.7%) alternated or combined with hypo pigmented areas (47.4%). This fact demonstrates an increase of melanin not only in skin and halo nevi but in dermal nevi too. A typical pigment network was seen only in 31.6% of patients, and a globular structure – in 50.5% of nevi. So, a new pattern was described - “post-globule circles” in 12.5% of nevi. However, due to the fact that the risk of malignancy affected by the disease and the therapy is not completely ruled out in this group, Vitiligo patients need a dynamic dermatoscopic examination to prevent and early diagnose the melanocyte dysplasia because this is an atypical dermatoscopic structure.
Conclusion
In conclusion, it is important to notice that depigmentation in patients with Vitiligo can be observed not only as skin patches, but also as a dermoscopic feature in melanocytic nevi, that is not any pathology nor any sign of dysplasia, but only a sign of the autoimmune reaction against the pigment.
Ethics, Consent and Permissions
This study was approved by Ethics committee. Written informed consent for participation in the study was obtained from all patients. There were no conflicts of interests.
References
- Workman M, Sawan K, Amm C (2013) Resolution and recurrence of vitiligo following excision of congenital melanocytic nevus. PediatrDermatol 30:166–168.
- Silveira M, Ferreira R, Alvarenga M, Mandelbaum S (2012) Association of giant congenital melanocytic nevus, halo nevus and vitiligo in a 75-year-old patient. An BrasDermatol87: 288–291.
- Concha-Garzón M,Hernández-Martín A, Faura-Berruga C, Dávila-Seijo P, Torrelo A, et al. (2014) Spontaneous partial repigmentation of halo nevi around congenital melanocytic nevus and vitiligo in a 13-year-old boy. Indian J DermatolVenereolLeprol80: 69–70.
- Sotiriou E, Apalla Z, Panagiotidou D, Ioannides D (2009) Partial pigmentary regression of a congenital nevocyticnaevus without halo phenomenon followed by generalized vitiligo. J EurAcadDermatol Venereol 23: 600–601.
- Ezzedine K, Diallo A, Léauté-Labrèze C, Séneschal J, Prey S, et al. (2012) Halo naevi and leukotrichia are strong predictors of the passage to mixed vitiligo in a subgroup of segmental vitiligo. Br JDermatol 166:539–544.
- Patrizi A, Bentivogli M, Raone B, Dondi A, Tabanelli M, et al. (2013) Association of halo nevus/I and vitiligo in childhood: A retrospective observational study. JEurAcadDermatol Venereol 27: 148–152.
- Wang P, Cheng Y, Yang H, Ran Y (2012) Acquired patch-type blue nevus with overlying vitiligo: A case report. Int JDermatol 51: 568–570.
- Luo X, Xu A, LiJ, Guan C (2010)Naevus of Ota associated with segmental vitiligo: A case report. J EurAcadDermatolVenereol 24: 611–612.
- Molochkov V (2005) Classification and characteristics of melanocytuc nevi (article in Russian). Estetic medicine 2: 266-270.
- Rezze G, Leon A, Duprat J (2011) Dysplastic nevus (atypical nevus). ActaDermVenereol91:428-431.
- Csoma Z, Erdei Z, Bartusek D (2008) The prevalence on melanocytic nevi among schoolchildren in South Hungary 22: 1412–1422.
- Hamzavi I, Lim H, Syed Z (2012) Ultraviolet-based therapy for vitiligo: what's new? Indian JDermatolVenereolLeprol 78:42-48.
- Goodson A, Grossman D (2009) Strategies for early melanoma detection: approaches to the patient with nevi. J Am Acad Dermatol 60 :719-735.
- Paradisi A, Tabolli S, Didona B, Sobrino L, Russo N, et al. (2014) Markedly reduced incidence of melanoma and non-melanoma skin cancer in a non-concurrent cohort of 10,040 patients with vitiligo. J Am AcadDermatol 71: 1110–1116.
- Teulings H, Overkamp M, Ceylan E, Nieuweboer-Krobotova L, et al. (2013) Decreased risk of melanoma and non-melanoma skin cancer in patients with vitiligo: A survey among 1,307 patients and their partners. Br JDermatol 168: 162–171.
- Teulings H, Overkamp M, Veen J (2013) Decreased risk of melanoma and non-melanoma skin cancer in patients with vitiligo: a survey among 1,307 patients and their partners. The British Journal of Dermatology 168:162-171.
- Newton B, Chang Y, Elliott F (2011) Relationship between sun exposure and melanoma risk for tumours in different body sites in a large case–control study in a temperate climate. Eur J Cancer47:732–741.
- Hammoud S, Kruis R, Sigurdsson V (2016) Prediction of the occurrence of melanoma and non-melanoma skin cancer in patients with vitiligo. ActaDermatoVenereologica96: 106–107.
- Piqué-Duran E, Palacios-Llopis S, Martínez-Martín M, Pérez-Cejudo J (2011) Complete regression of melanoma associated with vitiligo. DermatolOnline J17:4.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences